Enter to solve frequently given Mcqs (Detailed explanation present)
Question 1: With reference to infections with Escherichia coli the following are true except ?
A) Enteroaggregative E.coli is associated with Persistent diarrhoea
B) Enterohemorrhagic E.coli can cause haemolytic uraemic syndrome
C) Enteroinvasive E.coli produces a disease similar to salmonellosis
D) Enterotoxigenic E.coli is a common cause of traveler's diarrhoea
Answer: C
The pathogenic groups includes enterotoxigenic E. coli (ETEC), enteropathogenic E. coli (EPEC), enterohemorrhagic E. coli (EHEC), enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAEC), diffusely adherent E. coli (DAEC) and perhaps others that are not yet well characterized.
- Enterotoxigenic E. coli (ETEC) is a common cause of traveler's diarrhea and diarrhea in infants - both human and livestock. These strains usually encode adhesins (colonization factor antigens, or CFAs) that allow them to adhere to and colonize the intestinal epithelium. Once established, they secrete one or more toxins - one similar to cholera toxin - eliciting nausea, vomiting, abdominal cramps, and massive watery diarrhea leading to dehydration. In infants, the dehydration is often fatal if not treated.
- Enteroinvasive E. coli (EIEC) are able to invade and multiply within intestinal epithelial cells, resulting in cell destruction, intense inflammation, and ulceration of the intestinal lining. With symptoms of fever, cramps, vomiting, and bloody diarrhea, the disease closely resembles that caused by Shigella spp.
- Enteropathogenic E. coli (EPEC) cause diarrheal outbreaks and chronic diarrhea, especially in infants. After an initial association with intestinal epithelial cells, these strains elicit a response in the host cells resulting in the loss of microvilli and the formation of a platform, or pedestal, of actin fibrils at the site of bacterial attachment. The disease, manifesting as fever, vomiting, and a watery mucus-containing diarrhea, is associated with a limited number of E. coli serotypes. As with ETEC, the diarrhea can be fatal in infants and children, especially in developing countries.
- Enterohemorrhagic E. coli (EHEC) are similar to EPEC strains, but often produce severe illness including bloody diarrhea. These strains encode potent toxins similar if not identical to those of Shigella dysenteriae, which can cause the damage of intestinal epithelial cells, and interfere with protein biosynthesis in endothelial cells lining the microvasculature of the kidney and central nervous system. Among infected individuals, 2% to 7% develop hemolytic uremic syndrome (HUS), marked by red blood cell lysis and kidney failure. Fatality is common, especially among infants and the elderly. As with EPEC strains, EHEC are associated with a limited number of serotypes, and in the United States a single serological type, O157:H7, is the predominant representative.
- Enteroaggregative E. coli (EAEC) form aggregates of bacteria, many cells thick, which are quite distinct from the more isolated patches of bacterial cells typical of ETEC, EPEC, and EHEC strains. This aggregation may correlate with the persistent diarrhea caused by these strains.
- Diffusely adherent E. coli (DAEC), as the name suggests, form a much more dispersed association with host cells. They have been reported as being associated with diarrhea in some studies, but not in others. They have also been implicated with recurrent urinary tract infections.
Question 2: The following statements are true regarding melioidosis except ?
A) It is caused by Burkholderia mallei
B) The agent is a gram negative aerobic bacteria
C) Bipolar staining of the aetiological agent is seen with methylene blue stain
D) The most common form of melioidosis is pulmonary infection
Answer: A
- Melioidosis, also called Whitmore's disease, is an infectious disease caused by the bacterium Burkholderia pseudomallei. Melioidosis is clinically and pathologically similar to glanders disease, but the ecology and epidemiology of melioidosis are different from glanders. Melioidosis is predominately a disease of tropical climates, especially in Southeast Asia where it is endemic.
- Burkholderia pseudomallei is an organism that has been considered as a potential agent for biological warfare and biological terrorism.
- It mostly infects adults with an underlying predisposing condition, mainly diabetes mellitus.
There are 4 disease categories and these are the :
1. Acute Localized Infection: This form of infection is generally localized as a nodule and results from inoculation through a break in the skin. Studies in Thailand have shown suppurative parotitis to account for 38-40% of localized melioidosis in children.The acute form can produce fever and generalized muscle tenderness and may progress rapidly to infect the bloodstream.
2. Acute Pulmonary Infection: The lung is the most common organ affected.This form of the disease can produce a clinical picture ranging from mild bronchitis to severe pneumonia. A high fever (usually >39ºC), headache, anorexia and generalized muscle soreness typically accompany the onset of pulmonary melioidosis. Pleuritic or dull aching chest pain is common but a non-productive or productive cough with normal sputum is the hallmark of this form of melioidosis.
Radiologic findings include nodule, upper lobe consolidation, necrotizing lesions, thin walled cysts, cavitary lesions, pleural effusion, thickening or mediastinal abscess. Acute pulmonary infection is followed by the appearance of visceral abscesses and death with in a few days if left untreated. Almost every organ can be affected by melioidosis but the spleen is the most common extrapulmonary organ involved.
3. Acute Bloodstream Infection/Septicemic/Disseminated Melioidosis: Patients with underlying illness such as HIV, renal failure and diabetes mellitus are affected by this type of the disease, which usually results in septic shock.The symptoms vary depending on the site of the original infection but they generally include respiratory distress, severe headache, fever, diarrhea, and development of pus-filled lesions in the skin, muscle tenderness and disorientation. Sometimes there are signs of arthritis or meningitis.
Liver and spleen may be palpable. Liver function tests are often abnormal. WBC count may be normal to increased. The septicemic type is also rapidly fatal and displays a high mortality rate (up to 50%) when similarly left untreated. Many patients moribund on hospital admission die within 48 hours.
4. Chronic Suppurative Infection: It involves the organs of the body particularly of the reticuloendothelial system (liver/lung/spleen) or lymph nodes although any organ may be involved. Prognosis is poor when pneumonia occurs. It is more commonly found in whites than Asians. It may become dormant with exacerbation occurring years after primary infection when host defenses are impaired as a result of steroid, burns, DM or other processes .
- Gram stain may reveal small, gram-negative bacilli, which stain irregularly with methylene blue or Wright stain, and they may demonstrate a safety pin bipolar appearance.
- Ashdown's medium is a selective culture medium for the isolation and characterisation of Burkholderia pseudomallei.The medium contains crystal violet and gentamicin as selective agents to suppress the growth of other bacteria. Colonies of B. pseudomallei also take up neutral red which is present in the medium, and this further helps to distinguish it from other bacteria. Gentamicin slightly inhibits the growth of B. pseudomallei and so specimens inoculated onto Ashdown's agar needs to be incubated for a minimum of 96 hours instead of 48 hours. The medium is also enriched with 4% glycerol, which is required by some strains of B. pseudomallei to grow. B. pseudomallei usually produces flat wrinkled purple colonies on Ashdown's agar.
- The treatment of choice in patients with disseminated melioidosis is parenteral ceftazidime. Since relapse with melioidosis is common, treatment with an oral antibiotic such as doxycycline or cotrimoxazole should be continued for at least 2 months
Question 3: The following bacteria are most often associated with acute neonatal meningitis except ?
A) Escherichia coli
B) Streptococcus agalactiae
C) Neisseria meningitidis
D) Listeria monocytogenes
Answer: C
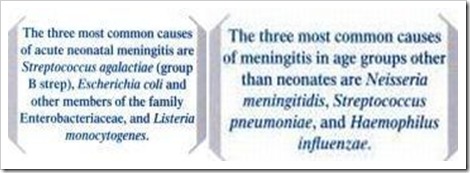
Question 4: All of the following Vibrio sp. are halophilic, except ?
A) V.cholerae
B) V.parahaemolyticus
C) V.alginolyticus
D) V.vulnifucus
Answer: A
All members of the genus are highly motile, facultatively anaerobic, curved gram-negative rods with one or more polar flagella. Except for V. cholerae and V. mimicus, all require salt for growth ("halophilic vibrios").
Question 5: All of the following organisms are known to survive intracellularly except ?
A) Neisseria meningitides
B) Salmonella typhi
C) Streptococcus pyogenes
D) Legionella pneumophila
Answer: C
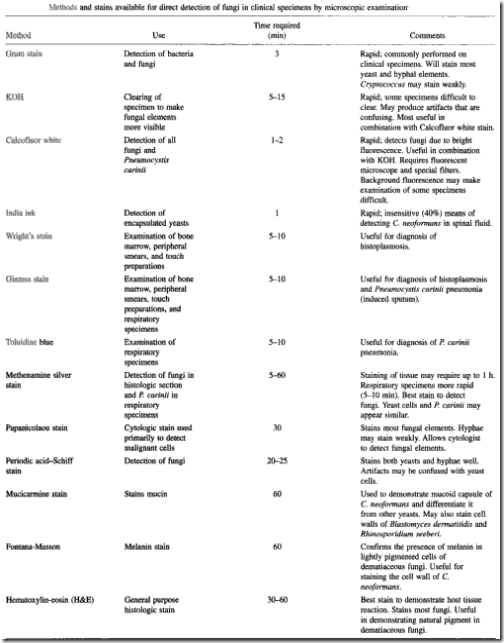
Question 6: The capsule of Cryptococcus neoformans in a CSF sample is best seen by ?
A) Grams stain
B) India ink preparation
C) Giemsa stain
D) Methanamine - Silver stain
Answer: B
An India ink preparation is commonly used with CSF to identify the organism and to support a presumptive diagnosis.
for histopathologic diagnosis of tissue samples:
- In tissue specimens, C neoformans is difficult to observe with routine hematoxylin and eosin stains.
- Use methenamine silver or periodic acid-Schiff stains to clearly demarcate C neoformans and to permit recognition of its characteristic shape and size, identifying it as a yeast-shaped organism that reproduces by the formation of narrow-based buds.
- cryptococcal yeast cell (but not the capsule) is stained by Gomori methanamine silver stain & periodic acid-Schiff stains
- Other stains that can be used to identify C neoformans include the Mayer mucicarmine stain & alcian blue which preferentially stains mucopolysaccharides and Masson-Fontan silver stain to detect melanin precursors in the yeast cell wall, which is also useful in differentiating C neoformans from other yeasts.
| Cause of meningitis | CSF Stain Findings for Selected Meningitis Causes |
| Cryptococcus neoformans | India ink stain shows typical encapsulated yeast forms |
| Haemophilus influenzae | Gram stain reveals gram-negative bacilli |
| Listeria monocytogenes | Difficult to diagnose; Gram stain may show gram-positive rods and/or coccobacilli |
| Neisseria meningitidis | Gram stain reveals gram-negative diplococcus |
| Streptococcus pneumoniae | Gram stain reveals gram-positive cocci in pairs |
Question 7: Viruses can be isolated from clinical samples by cultivation in the following except ?
A) Tissue culture
B) Embryonated eggs
C) Animals
D) Chemically defined media
Answer: D
Question 8: It is true regading the normal microbial flora present on the skin and mucous membranes that ?
A) It cannot be eradicated by antimicrobial agents
B) It is absent in the stomach due to the acidic pH
C) It establishes in the body only after the neonatal period
D) The flora in the small bronchi is similar to that of the trachea
Answer: B
Question 9: An army jawan posted in a remote forest area had fever and headache. His fever was 104°F and pulse was 70 per min. He had an erythematous lesion of about 1 cm on the leg surrounded by small vesicles, along with generalized lymphadenopathy at the time of presentation to the referral hospital. His blood sample was collected to perform serology for the diagnosis of Rickettsial disease. Which one of the following results in Weil-felix reaction will be diagnostic in this clinical setting ?
A) High OX-2
B) High OX-19
C) High OX-K
D) High OX-19 and OX-2
Answer: C
- This is a case of scrub typhus(chigger-borne typhus) with classical clinical presentaqtion.
- The classic case description includes an eschar at the site of chigger feeding, regional lymphadenopathy, and a maculopapular rash.
- After an incubation period of 6 to 21 days (usually 8 to 10 days), the onset of disease is characterized by fever, headache, myalgia, cough, and gastrointestinal symptoms.
- Severe cases typically include prominent encephalitis and interstitial pneumonia as key features of vascular injury.
| disease | Agglutination pattern with OX 19 | with OX 2 | with OX K |
| epidemic typhus | +++ | + | - |
| Brill-zinsser disease | usually negative or week positive | usually negative or week positive | - |
| endemic typhus | +++ | +/- | - |
| tickborne spotted fever | ++ | ++ | - |
| scrub typhus | - | - | +++ |
Question 10: Adenosine deaminase (enzyme) deficiency is associated with ?
A) Severe combined immunodeficiency (SCID)
B) X-linked agammaglobulinemia
C) Transient hypogammaglobulinemia of infancy
D) Chronic granulomatous disease
Answer: A
- SCID, Severe Combined Immunodeficiency, is a primary immune deficiency. The defining characteristic is usually a severe defect in both the T- & B-lymphocyte systems.
- SCID is often called "bubble boy disease"
- There are several forms of SCID. The most common type is linked to the X chromosome, making this form affect only males. Other forms of SCID usually follow an autosomal recessive inheritance pattern or are the result of spontaneous mutations. One of these other forms is linked to a deficiency of the enzyme adenosine deaminase (ADA). Other cases of SCID are caused by a variety of other defects.
Adenosine deaminase catalyses the conversion of adenosine to inosine & is released by macrophages & lymphocytes during the cellular immune response.increased ADA levels are used in diagnosis of Tuberculosis pleural effusion.
The pleural fluid ADA values can be used in conjunciton with cell counts, in the following way:
1- A lymphocyte exudate (lymphocytes to neutrophils ratio) (L/N ratio >0.75) with a high ADA value (> 50 U/L) is highly suggestive of TB pleurisy.
2- A lymphocyte exudate with low ADA value (<50 U/L) is suggestive of nonhematologic malignancies.
3- A neutrophilic exudate (L/N <0.75) with a high ADA concentration (>50 U/L) is suggestive of parainfective effusions
- ADA estimation in CSF is a simple,inexpensive, rapid and fairly specific method for aiding a clinician in making the diagnosis of tuberculous meningitis when confronted with a common dilemma of distinguishing it from partially treated pyomeningitis and other meningities.
- ADA level of 4 U/l and above could provide additional supportive evidence for the diagnosis of TBM in clinically suspected and bacteriologically negative cases
Question 11: Which of the following viral infections is transmitted by tick ?
A) Japanese encephalitis
B) Dengue fever
C) Kyasanur forest disease (KFD)
D) Yellow fever
Answer: C
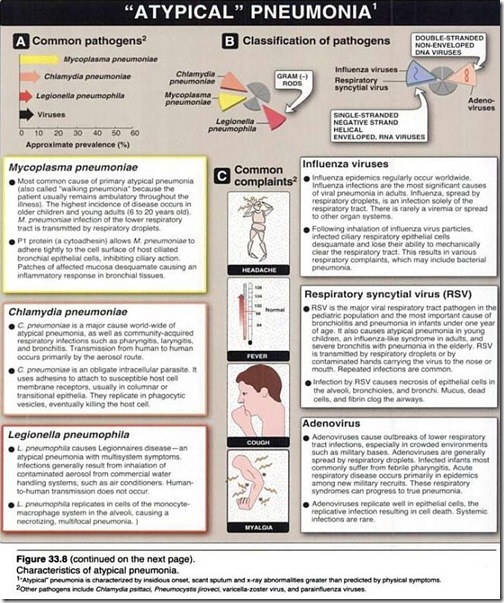
Question 12: Atypical pneumonia can be caused by the following microbial agents except ?
A) Mycoplasma pneumoniae
B) Legionella pneumophila
C) Adeno virus
D) Klebsiella pneumoniae
Answer: D
Question 13: The serum concentration of which of the following human IgG subclass is maximum ?
A) IgG1
B) IgG2
C) IgG3
D) IgG4
Answer: A
There are four IgG subclasses (IgG1, 2, 3 and 4) in humans, named in order of their abundance in serum (IgG1 being the most abundant).
| subclass | Percent | Crosses placenta easily | Complement activator | Binds to Fc receptors on phagocytic cells |
| IgG1 | 65% | yes | second highest | high affinity |
| IgG2 | 23% | no | third highest | extremely low affinity |
| IgG3 | 8% | yes | highest | high affinity |
| IgG4 | 4% | yes | no | intermediate affinity |
Question 14: Chlamydia trachomatis is associated with the following except ?
A) Endemic trachoma
B) Inclusion conjunctivitis
C) Lymphogranuloma venereum
D) Community acquried pneumonia
Answer: D
Chlamydia. C trachomatis can be differentiated into 18 serovars (serologically variant strains) based on monoclonal antibody–based typing assays.
- Serovars A, B, Ba, and C are associated with trachoma (a serious eye disease that can lead to blindness),
- serovars D-K are associated with genital tract infections, and
- L1-L3 are associated with lymphogranuloma venereum ([LGV]
Question 15: The following statements are true regarding Clostridium perfringens except ?
A) It is the commonest cause of gas gangrene
B) It is normally present in human faeces
C) The principal toxin of C.perfringens is the alpha toxin
D) Gas gangrene producing strains of C.perfringens produce heat resistant spores
Answer: D
Clostridia are present in the normal colonic flora. C. ramosum is the most common and is followed in frequency by C. perfringens in colonizing clostridium. While most common colonizing organisms in colon are bacteriods.
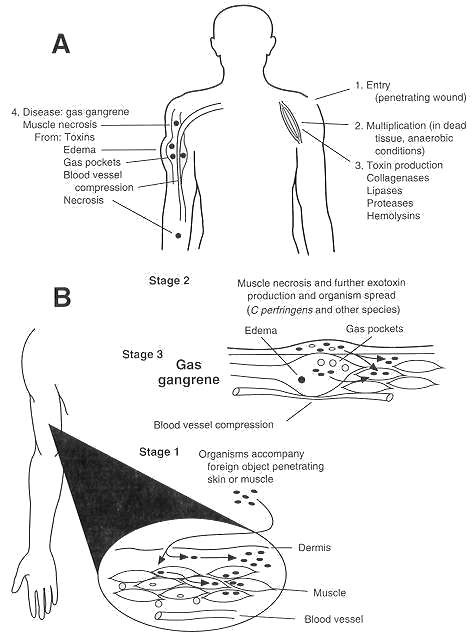
Gas gangrene is an acute disease with a poor prognosis and often fatal outcome Initial trauma to host tissue damages muscle and impairs blood supply. This lack of oxygenation causes the oxidation-reduction potential to decrease and allows the growth of anaerobic clostridia. Initial symptoms are generalized fever and pain in the infected tissue. As the clostridia multiply, various exotoxins (including hemolysins, collagenases, proteases, and lipases) are liberated into the surrounding tissue, causing more local tissue necrosis and systemic toxemia. Infected muscle is discolored (purple mottling) and edematous and produces a foul-smelling exudate; gas bubbles form from the products of anaerobic fermentation. As capillary permeability increases, the accumulation of fluid increases, and venous return eventually is curtailed. As more tissue becomes involved, the clostridia multiply within the increasing area of dead tissue, releasing more toxins into the local tissue and the systemic circulation. Because ischemia plays a significant role in the pathogenesis of gas gangrene, the muscle groups most frequently involved are those in the extremities served by one or two major blood vessels
- In gas gangrene the primary pathogen can be any one of various clostridial species including C perfringens (80%), C novyi (40%), C septicum (20%), and, occasionally, C bifermentans, C histolyticum, or C fallax.
- Isolation of 107 or more clostridia per milliliter of wound exudate is strong evidence for a clostridial wound infection.
- Clostridium perfringens is classified into 5 types (A–E) on the basis of its ability to produce one or more of the major lethal toxins, alpha, beta, epsilon and iota (α, β, ε, and ι)
- Alpha-toxin (a lecithinase, also called phospholipase-C) and theta-toxin (oxygen-labile cytolysin) are both considered important in the disease pathology.
- A commonly used laboratory test for presumptive identification of C perfringens is the Nagler reaction which detects the presence of alpha-toxin (phospholipase-C), one of the most prominent toxins produced by C perfringens.
- C perfringens type A is a major cause of food poisoning
- C perfringens, usually type C also causes Necrotizing enteritis in human
- Gas gangrene producing strains of C. perfringens produce heat labile spores and get destroyed with boiling.But those of 'food poisoning strains' of Type A & certain Type C strains resist boiling for 1-3 hours.
Question 16: The most common organism amongst the following that causes acute meningitis in an AIDS patient is ?
A) Stretococus pneumoniae
B) Streptococcus agalactiae
C) Cryptococcus neoformans
D) Listeria monocytogenes
Answer: C
- Pneumocystis carinii is the most frequent opportunistic infection seen with AIDS. It produces a pulmonary infection, called Pneumocystis carinii pneumonia (PCP), but rarely disseminates outside of lung.
- Candidiasis is most common fungal infection in patients with AIDS.Candida infection of oral cavity (thrush)& esophagus are the two most common clinical manifestations in HIV infected individuals
- Meningitis is the major clinical manifestation of cryptococcosis .(second common fungal infection)
- Cytomegalovirus (CMV) is the most frequent disseminated opportunistic infection seen with AIDS. It causes the most serious disease as a pneumonia in the lung, but it can also cause serious disease in the brain and gastrointestinal tract. It is also a common cause for retinitis and blindness in persons with AIDS.
Question 17: A bacterial disease that has been associated with the 3 "Rs" i.e., rats, ricefields, and rainfall is ?
A) Leptospirosis
B) Plague
C) Melioidosis
D) Rodent-bite fever
Answer: A
• Leptospirosis is a zoonosis with a worldwide distribution. Water is an important vehicle in their transmission. Epidemics of leptospirosis may result from exposure to flood waters contaminated by urine from infected animals
• Leptrospira are excreted in urine of infected animals for a long time. Rats, mice and voles particularly R. novergicus and Mus musculus are Reservoirs.
• Human infection is usually caused by occupational exposure to the urine of infected animals, eg agricultural and live stock farmers, worker in rice fields.
• Leisure time activities such as swimming and fishing also carry risks.
• Leptospira shed in urine and can survive for weeks in soil and water heavy rainfall can leads to high level of contamination of soil of that area. Potential contamination of water occurs.
Question 18: A child was diagnosed to be suffering from diarrhoea due to Camplyobacter jejuni. Which of the following will be the correct enviornmental conditions of incubation of the culture plates of the stool sample ?
A) Temperature of 42°C and microaerophilic
B) Temperature of 42°C and 10% carbondioxide
C) Temperature of 37°C and microaerophilic
D) Temperature of 37°C and 10% carbondioxide
Answer: A
Identification of Campylobacter
Typical Campylobacter colonies are gray to pinkish or yellowish gray and slightly mucoid or “runny.” Suspicious colonies isolated from feces may be presumptively identified as Campylobacter spp. if they meet the following criteria:
•Growth at 42º C: C. jejuni spp. jejuni (the most common cause of bacterial gastroenteritis) and C. coli grow at 42º C; other colon bacteria are inhibited at this temperature.They are usually sensitive to O2 and super oxide, yet O2 is essential for growth, so micro-aerophilic condition must be provided for their cultivation.they also require 10% CO2.
•Oxidase and catalase positive : Most pathogenic Campylobacter species are oxidase and catalase positive.
•Characteristic curved morphology on Gram stain: Campylobacter species appear as faintly-staining gram-negative rods with a characteristic “seagull-wing” shape. However, they stain poorly with safranin, so carbolfuchsin is recommended as a counterstain. Or, if safranin is used, counterstaining should be extended to 2-3 minutes.
•Darting motility in wet preparation: Campylobacter species have a distinctive darting motility when observed in a wet preparation made from Brucella or trypticase soy broth. Distilled water or saline should not be used because these appear to inhibit motility.
Question 19: Which one of the following statements is true regarding Chlamydia pneumoniae ?
A) Fifteen serovars have been identified as human pathogens
B) Mode of transmission is by the airborne bird excreta
C) The cytoplasmic inclusions present in the sputum specimen are rich in glycogen
D) The group specific antigen is responsible for the production of complement fixing antibodies
Answer: D
- only one serotype present
- Person-to-person transmission by respiratory secretions.
- Pneumonia or bronchitis, gradual onset of cough with little or no fever.
- C. pneumoniae infection may be associated with atherosclerotic vascular disease.
- Chlamydia pneumoniae produces the glycogen negative inclusion bodies that are much like of Chlamydia psittaci and are sulfonamide-resistant.
- Serology using the Microimmuno-fluorescent test is the most sensitive method for the detection of Chlamydia pneumoniae infection. This test is the species specific not the complement fixing antibody detection by complement fixation test. Because the complement fixing antibodies are against the group specific antigen so detection of these antibodies are not species specific.
- Doxycycline is the treatment of choice except in children younger than 9 years and in pregnant women. Treatment should be continued for at least 10-14 days after defervescence.
- Telithromycin is the first antibiotic in a new class called ketolides and is approved for C pneumoniae pneumonia by the US Food and Drug Administration.Telithromycin is a potent inhibitor of CYP3A4 and can cause potentially dangerous increases in serum concentrations of simvastatin, lovastatin, atorvastatin, midazolam, and other drugs. If telithromycin is used, statins should be withheld for the duration of therapy. Hepatotoxicity has been reported. It is contraindicated in patients with myasthenia gravis.
Question 20: Which of the following is not a neuroparasite ?
A) Taenia solium
B) Acanthamoeba
C) Naegleria
D) Trichinella spiralis
Answer: D
| parasites Affecting the Central Nervous System | |
| Protozoa: | |
| Naegleria fowleri | acute primary amebic meningoencephalitis (PAM) |
| Acanthamoeba species | chronic granulomatous amebic encephalitis(GAE) |
| Balamuthia mandrillaris | sub-acute or chronic GAE |
| Entamoeba histolytica | Brain abscess |
| Trypanosoma gambiense T. rhodesiense | Sleeping sickness |
| T. cruzi | Neurological complications.(Chagas’ Disease) |
| Plasmodium falciparum | Cerebral malaria |
| Toxoplasma gondii | Encephalitis,Brain calcifications; Blindness |
| Trematodes | |
| Paragonimus spp Fasciola spp | Brain cysts |
| Schistosoma spp | Eggs/adults in CNS |
| Cestodes | |
| Taenia solium | neurocysticercosis |
| Echinococcus granulosus | Cerebral hydatid |
Question 21: Virus mediated transfer of host DNA from one cell to another is known as ?
A) Transduction
B) Transformation
C) Transcription
D) Integration
Answer: A
Question 22: HIV can be detected and confirmed by ?
A) Polymerase Chain Reaction (PCR)
B) Reverse Transcriptase - PCR
C) Real Time PCR
D) Mimic PCR
Answer: B
Question 23: In the small intestine, cholera toxin acts by ?
A) ADP-ribosylation of the G regulatory protein
B) Inhibition of adenyl cyclase
C) Activation of GTPase
D) Active absorption of NaCl
Answer: A
| TOXIN | ENZYMATIC ACTIVITY | BIOLOGICAL EFFECTS |
| Cholera toxin | ADP ribosylates eucaryotic adenylate cyclase Gs regulatory protein | Activates adenylate cyclase; increased level of intracellular cAMP promote secretion of fluid and electrolytes in intestinal epithelium leading to diarrhea |
| E. coli heat-labile toxin LT | ADP ribosylates adenylate cyclase Gs regulatory protein | Similar or identical to cholera toxin |
| Shiga toxin | Enzymatically cleaves eucaryotic 28S rRNA | results in inhibition of protein synthesis in susceptible cells. Results in diarrhea, hemorrhagic colitis (HC) and hemolytic uremic syndrome (HUS) |
| Diphtheria toxin | ADP ribosylates elongation factor 2 | Inhibits protein synthesis in animal cells resulting in death of the cells |
| Pseudomonas Exotoxin A | ADP ribosylates elongation factor-2 analogous to diphtheria toxin | Inhibits protein synthesis in susceptible cells, resulting in death of the cells |
| Pertussis toxin | ADP ribosylates adenylate cyclase Gi regulatory protein | the Gi protein is inactivated and cannot perform its normal function to inhibit adenylate cyclase. The conversion of ATP to cyclic AMP cannot be stopped.increased levels of cAMP affect hormone activity and reduce phagocytic activity |
| Botulinum toxin | Zn++ dependent protease acts on synaptobrevin at motor neuron ganglioside | Inhibits presynaptic acetylycholine release at neuromuscular synapses resulting in flaccid paralysis |
| Tetanus toxin | Zn++ dependent protease acts on synaptobrevin in central nervous system | Inhibits neurotransmitter release from inhibitory neurons in the CNS resulting in spastic paralysis |
3 comments:
Here is a great herbal doctor who cured me of Hepatitis B. his name is Dr. Imoloa. I suffered Hepatitis B for 11 years, I was very weak with pains all over my body my stomach was swollen and I could hardly eat. And one day my brother came with a herbal medicine from doctor Imoloa and asked me to drink and I drank hence there was no hope, and behold after 2 week of taking the medicine, I started feeling relief, my swollen stomach started shrinking down and the pains was gone. I became normal after the completion of the medication, I went to the hospital and I was tested negative which means I’m cured. He can also cure the following diseases with his herbal medicine...lupus, hay fever, measles, dry cough, diabetics hepatitis A.B.C, mouth ulcer, mouth cancer, bile salt disease, fol ate deficinecy, diarrhoea, liver/kidney inflammatory, eye cancer, skin cancer disease, malaria, chronic kidney disease, high blood pressure, food poisoning, parkinson disease, bowel cancer, bone cancer, brain tumours, asthma, arthritis, epilepsy, cystic fibrosis, lyme disease, muscle aches, fatigue, muscle aches, shortness of breath, alzhemer's disease, acute myeloid leukaemia, acute pancreatitis, chronic inflammatory joint disease, Addison's disease back acne, breast cancer, allergic bronchitis, Celia disease, bulimia, congenital heart disease, cirrhosis, constipation, fungal nail infection, fabromyalgia, (love spell) and many more. he is a great herbalist man. Contact him on email; drimolaherbalmademedicine@gmail.com. You can also reach him on whatssap- +2347081986098.
My name is hoover, my 18 year old daughter, Tricia was diagnosed with herpes 3 years ago. Since then, we have moved from one hospital to another. We tried all kinds of pills, but every effort to get rid of the virus was futile. The bubbles continued to reappear after a few months. My daughter was using 200mg acyclovir pills. 2 tablets every 6 hours and 15g of fusitin cream. and H5 POT. Permanganate with water to be applied twice a day, but all still do not show results. So, I was on the internet a few months ago, to look for other ways to save my only son. Only then did I come across a comment about the herbal treatment of Dr Imoloa and decided to give it a try. I contacted him and he prepared some herbs and sent them, along with guidance on how to use them via the DHL courier service. my daughter used it as directed by dr imoloa and in less than 14 days, my daughter recovered her health. You should contact dr imoloa today directly at his email address for any type of health problem; lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis ABC, syphilis, diarrhea, HIV / AIDS, Huntington's disease, back acne, chronic kidney failure, addison's disease, chronic pain, Crohn's pain, cystic fibrosis, fibromyalgia, inflammatory Bowel disease, fungal nail disease, Lyme disease, Celia disease, Lymphoma, Major depression, Malignant melanoma, Mania, Melorheostosis, Meniere's disease, Mucopolysaccharidosis, Multiple sclerosis, Muscular dystrophy, Rheumatoid arthritis Alzheimer's disease, parkinson's disease, vaginal cancer, epilepsy Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumor, Malignant, Bruxism, Bulimia, Cervical Disc Disease, Cardiovascular Disease, Neoplasms , chronic respiratory disease, mental and behavioral disorder, Cystic Fibrosis, Hypertension, Diabetes, Asthma, Autoimmune inflammatory media arthritis ed. chronic kidney disease, inflammatory joint disease, impotence, alcohol spectrum feta, dysthymic disorder, eczema, tuberculosis, chronic fatigue syndrome, constipation, inflammatory bowel disease. and many more; contact him at drimolaherbalmademedicine@gmail.com./ also with whatssap- + 2347081986098.
I started on COPD Herbal treatment from Ultimate Health Home, the treatment worked incredibly for my lungs condition. I used the herbal treatment for almost 4 months, it reversed my COPD. My severe shortness of breath, dry cough, chest tightness gradually disappeared. Reach Ultimate Health Home via their website www.ultimatelifeclinic.com . I can breath much better and It feels comfortable!
Post a Comment