These 3 tests are non-specific & they don't indicate the type of deafness.they only give a rough idea about the hearing loss.
| Finger friction test | rubbing or snapping thumb & finger close to patients ear |
| Watch test | clicking watch brought near the patients ear |
| Speech test | patient stands with his test ear towards examiner at distance of 6metres. |
Tuning fork tests:remember these ,its very important
- 512Hz tuning fork is ideal(forks of lower frequency - produce sense of bone vibration forks of higher frequency- shorter decay time )
- When we test air conduction ,we actually check the functioning of both conductive & sensorineural(cochlea)
- When we test Bone conduction ,we actually measure only cochlear function
- Normally hearing through air conduction is louder & heard twice as long as through bone conduction route(AC better than BC)
Rinne test:
method:To perform this test, a 512Hz vibrating tuning fork is placed on the mastoid bone and then moved next to the external ear. The patient indicates at which of the two sites the sound is louder.
 principle:Sound transmitted through an external ear traverses the middle ear and is perceived by the cochlea (inner ear). Sound can be transmitted directly to the cochlea, skipping the external and middle ear, by placing the vibrating tuning fork on the mastoid bone directly behind the ear. This is the basis for the Rinne hearing test.
principle:Sound transmitted through an external ear traverses the middle ear and is perceived by the cochlea (inner ear). Sound can be transmitted directly to the cochlea, skipping the external and middle ear, by placing the vibrating tuning fork on the mastoid bone directly behind the ear. This is the basis for the Rinne hearing test.
| normal | conductive deafness | SN deafness |
| Rinne | AC>BC
(Rinne +) | BC>AC
(Rinne -) | AC>BC |
note:
| rinne (-)ve | 256Hz fork | 512Hz fork | 1024Hz fork |
minimum
air-bone gap | 15dB | 30dB | 45dB |
False negative Rinne :
- in Severe Unilateral sensorineural hearing loss.
- Patient does not perceive sound by air conduction ,but responds to bone conduction
- response to bone conduction is because the patient perceives sound from opposite ear because of transcranial transmission of sound.
- corrected by :masking opposite ear with Barany's noise box ,so that transcranial transmission of sound is not perceived.

note:A Barany noise box can also be used to see noise based vertigo (Tullio phenomenon). This commercially available box simply makes a loud (100 dB) noise. When the box is slowly moved towards the patient's symptomatic ear, the vertiginous symptoms may be re-created.
Weber test:
method:Place the tuning fork in the center of the forehead and the physician asks the patient where he or she hears it.
principle:
- The occlusion effect is responsible for this phenomenon. Sound conducted through bone causes the cochlea, the ossicular chain, and the air in the external auditory canal to vibrate. Some lower frequency sound, as produced by the 512 Hz tuning fork, escapes from the canal. When the ear is occluded, these frequencies cannot escape and the sound seems to become louder.
- it is the occlusion effect, rather than elimination of environmental sound, that is responsible for the improved bone conduction threshold when occluding a normal ear.
- Middle ear effusion and ossicular chain disruptions cause a "mass loaded" middle ear, with lowering of the inherent resonant frequency. Ossicular chain fixation causes a phase shift in the sound wave. Both cause preferential transmission of lower frequencies to the cochlea
| normal | conductive deafness | SN deafness |
| Weber | not lateralised | lateralised to poorer ear | lateralised to better ear |
note:lateralisation of sound in Weber test with a tuning fork of 512Hz implies either
- conductive loss of 15-20dB in ipsilateral ear (or)
- sensorineural deafness in contralateral ear
Absolute bone conduction test(ABC) test:
method:
patients bone conduction compared to that of examiner(presuming that examiner has normal hearing)by keeping on mastoid.
External auditory meatus of both patient & examiner is occluded by pressing tragus inwards ,this is to prevent external ambient noise entering through air conduction route.
| normal | conductive deafness | SN deafness |
| ABC test | hear the fork for same duration as examiner | hear the fork for same duration as examiner. | reduced |
Schwabach test:
method:same as ABC test,but meatus is not occluded.
| normal | conductive deafness | SN deafness |
| Schwabach | equal | lengthened in patient(due to absence of external ambient noise the patient hears it for longer time) | reduced |
Bing test::
determine whether closing of ear canal results in occlusion effect.
The Bing test can simulate unilateral (one-sided) conductive hearing loss results by placing a finger in one ear while performing the Weber test.
method:tuning fork placed on mastoid while examiner alternately closes & opens ear canal by pressing tragus inwards.
principle:same principle as Weber test(occlusion effect)
| normal | conductive deafness | SN deafness |
| Bing test | louder(when occluded) | no effect
(bing negative) | louder |
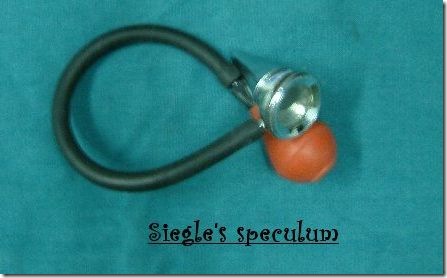
Gelle's test:
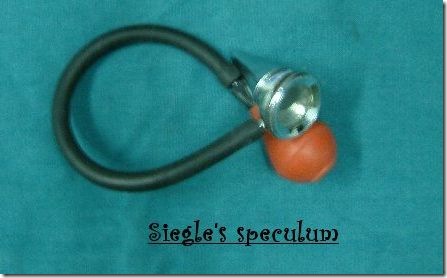
method:A vibrating tuning fork is applied over the mastoid process; if it is heard, the air in the external auditory canal is compressed, by means of a Siegle's speculum.
a test of the mobility of the ossicles.
principle:
- when air pressure is increased in ear canal, it pushes tympanic membrane inside & leading to increased stiffness of the ossicular chain & thus decreases hearing.
- And when pressure is again released ,it again normalises.
| normal | stapes fixation(otosclerosis) | SN deafness |
| Gelle's test | decreased in intensity after increasing pressure | does not alter | decreased in intensity after increasing pressure |
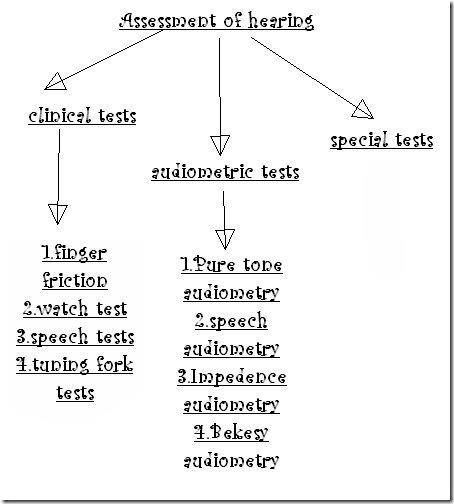
Audiometric tests:
Pure tone audiometry:
- used to measure the auditory threshold of an individual
- pure tone-a single frequency sound is used while testing ,audiometer-an electronic device which produces pure tones.
Audiometer: There are two types of audiometers widely used. They are:
1. Those that require a subjective response on the part of the patient and
2. Those that require no subjective response from the patient.
Examples include:
1. Pure tone audiometer is the classic example of the first type
2. Impedence audiometer / BERA (Brainstem Auditory Evoked Responses audiometer) are examples of the second type.
- The frequencies generated are 125, 250, 500,750, 1000, 1500, 2000, 3000, 4000, 6000 and 8000 Hz.
- Intensity is the level of sound power measured in decibels; loudness is the perceptual correlate of intensity.
- Frequency is cycles per unit of time. Pitch is the perceptual correlate of frequency. Frequency is measured in hertz, which are cycles per second.
- Usually frequencies of 250-8000 Hz are used in testing because this range represents most of the speech spectrum, although the human ear can detect frequencies from 20-20,000 Hz.
- The hearing level (HL) is quantified relative to "normal" hearing in decibels (dB), with higher numbers of dB indicating worse hearing. The dB score is not really percent loss, but neverthless 100 dB hearing loss is nearly equivalent to complete deafness for that particular frequency. A score of 0 is normal. It is possible to have scores less than 0, which indicate better than average hearing.
- note:In a normal PTA audiogram we see that both AC(air conduction) & BC(bone conduction) are at the same 0dB level.But we know that AC is better than BC.So you may get a doubt how come they are same here.Actually In a clinic a calibrated audiometer is used to present the correct intensity for each tone such that 'normal hearing' registers as 0 dB HL (audiometric zero) .This is done for the ease of reading the audiogram report.& standardisation
- 0 dB Hearing Level at 1000 Hz = 7 dB SPL
Pure tone air conduction testing:
This is a measurement of air conduction thresholds of audibility.
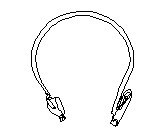
Pure tone air conduction threshold is tested using head phones:
method:
note:when establishing threshold ,2 choices are ascending & descending way to change intensity.
- ascending(Hughson - Westlake ascending technique)- begins with stimuli that are below patient's threshold & intensity is increased until patient responds.
- descending- stimuli presented first are above patient's threshold & intensity is decreased until the patient no longer responds.
but both have drawbacks=
- in descending technique the patient might continue to respond to stimuli ,when he no longer perceives (false + response)
- in ascending technique the patient may fail to respond even when stimuli are audible.(false - response)
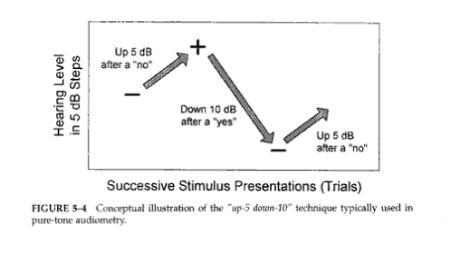
Modified Hughson - Westlake technique :this procedure uses an ascending technique to determine threshold .but each threshold search is preceeded by a descending familiarization trial.
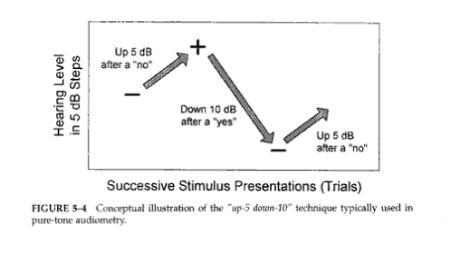
ex:"Up 5-down 10" method of threshold estimation
- The better ear is tested first in order to determine the need for masking.
- Start with a 1000 Hz tone at a level above the threshold to allow easy identification of the tone. This tone is selected because it is an important speech frequency, and the patient is less apt to mistake the frequency. To ensure the subject is familiar with the task, present a tone of 1000 Hz that is clearly audible (e.g. at 40 dB HL for a normally hearing subject or approximately 30 dB above the estimated threshold for a subject with a hearing impairment,)
- If the patient is suspected to be having a profound hearing loss then the testing should be started with 250Hz frequency. This is because of the fact that the individuals with profound hearing loss often have testable hearing only in the low frequency range.
- Next, test 2000, 4000, 8000, 500 and 250 Hz in that order
- As the threshold levels are being reached, a check should be made for the existance of abnormal tone decay. This is done by sustaining the tone for several seconds longer than usual. If the index finger drops before the tone is discontinued, abnormal tone decay should be suspected.
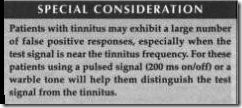
- "Up 5-down 10" method =The starting intensity of the test tone is reduced in 10 dB steps following each positive response, until a hearing threshold level is reached at which the subject fails to respond. Then, the tone is raised by 5 dB, if the subject hears this increment, the tone is reduced by 10 dB; if the tone is not heard then ti is raised by another 5 dB increment. This 5 dB increment is always used if the preceding tone is not heard, and a 10 dB decrement is always used when the sound is heard. The threshold is defined as the faintest tone that can be heard 50% or more of the time, and is established after several threshold crossings.
- Testing of the second ear should begin with the last frequency used to test the first ear. There is no need to start again with a 1000 Hz tone because if one side of the heard has learned the listening task, the other side knows it as well. The test is terminated after all desired frequencies have been examined.
Bone conduction audiometry:
This is an important measurement of hearing threshold using a bone vibrator. This helps to differentiate conductive from sensorineural hearing loss. The equipment necessary is just a bone vibrator connected to the audiometer. The bone vibrator is placed over the mastoid process of the side to be tested. The auditory threshold is assessed as described for air conduction assessment. The only difference is that the better hearing ear should be masked using a masking tone delivered via a head phone.
Limitations of bone vibrators
- Bone vibrators tend to emit more sound than vibration at frequencies above 2000 Hz If testing at 3000 and 4000 Hz it is preferable to insert an ear plug (eg E.A.R. plug as used for hearing protection purposes) into the test ear canal or cover the test ear with a supra-aural earphone. This attenuates the air borne radiation from the bone vibrator to a satisfactory degree. Failure to occlude the ear canal at high test frequencies is likely to lead to inaccurately acute bone conduction thresholds, resulting in a false air-bone gap in the audiometric results. The canal must not be occluded at test frequencies below 3000 Hz since this may produce the “occlusion effect” in which bone conduction thresholds are improved.
- Testing is not recommended at frequencies below 500 Hz because the subject’s threshold may relate to hearing at the second or third harmonic rather than the fundamental.
- In bone conduction audiometry high frequencies cannot be used for testing. Frequencies above 4000 Hz cannot be used because they are beyond the vibrating capabilities of the bone vibrator.
Masking
- Masking presents a constant noise to the nontest ear to prevent crossover from the test ear. The purpose of masking is to prevent the nontest ear from detecting the signal (line busy), so only the test ear can respond.
- When a signal is presented to the test ear, the signal may also travel through the head and reach the cochlea on the other side. However the intensity of the signal from the test to the nontest ear can be reduced by the mass of the head. This signal reduction is called interaural attenuation.(‘transcranial transmission loss’)
- For bone conduction, the interaural attenuation may be as low as 0 dB because the bones of the skull are very efficient at transmitting sound. Thus, any suspected difference in bone conduction between the test and nontest ears requires masking. (ie,Masking is done in all Bone conduction studies)
- Crossover occurs when sound presented to the test ear travels across the head to the nontest ear. This occurs at approximately 40 dB for circumaural earphones across all frequencies.Interaural attenuation for air conduction can range between 40 and 80 dB. Masking should be used if the difference in air conduction in one ear and bone conduction in the other ear is 40 dB or greater.(ie,masking required when there is difference b/w the 2 ears of minimum 40dB in air conduction threshold )
- When the difference in the thresholds of the two ears is greater than the transcranial transmission loss, cross-hearing may occur and the apparent threshold of the worse ear is in fact a ‘shadow’ of the better ear.
- Narrow band masking noise is used
Audiograms:
- red indicates right ear
- blue indicates left ear.

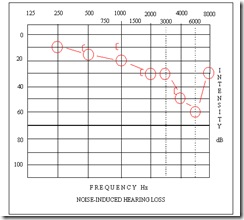
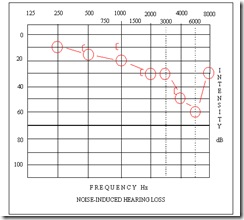
eg: high-frequency sensorineural hearing loss in the right ear.
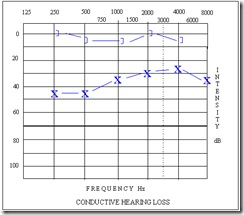
Audiogram depicting a mild rising conductive hearing loss in the left ear:
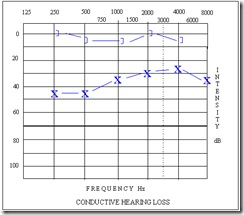
The 3 types of hearing loss can be differentiated as follows:
- Conductive hearing loss has normal bone-conduction thresholds, but air-conduction thresholds are poorer than normal by at least 10 dB.
- Sensorineural hearing loss has bone- and air-conduction thresholds within 10 dB of each other, and thresholds are higher than 25 dB HL.
- Mixed hearing loss has conductive and sensorineural components.Pure-tone air-conduction thresholds are poorer than bone-conduction thresholds by more than 10 dB, and bone-conduction thresholds are less than 25 dB
Speech audiometry:
- test patient's ability to hear & understand speech is measured.
- different parameters are measured like:
(a)speech recognition threshold :Speech reception threshold:or Spondee threshold
- minimum intensity at which 50% of words repeated correctly by patient.
- Spondee words are used.Spondees are two syllable words with equal accent (emphasis) on each syllable. Baseball, northwest, oatmeal and hotdog are examples of spondees.
- The term speech recognition threshold is synonymous with speech reception threshold. Speech recognition threshold is the preferred term because it more accurately describes the listener's task.
- SRT should be within 10dB of PTA.(since SRT encompasses far more frequencies than PTA , SRT is less than PTA )
- If the SRT is significantly better than the PTA, the possibility of pseudohypoacusis(patient is not co-operating properly) should be considered
- note:Pure tone average(PTA)=average of pure tone threshold of 3 separate frequencies (500 ,1000 ,2000Hz) as measured by pure tone audiometry.
(b)Speech detection threshold:
- Speech-awareness threshold (SAT) is also known as speech-detection threshold (SDT).
- The objective of this measurement is to obtain the lowest level at which speech can be detected at least half the time. This test does not have patients repeat words; it requires patients to merely indicate when speech stimuli are present.
- Speech materials usually used to determine this measurement are spondees
note:SRT differs from SDT in that SDT is merely the level at which the individual becomes aware that speech is present & SRT is level at which speech is loud enough for the individual to understand it.
(c)speech recognition score :
- Speech discrimination score or word recognition score(when words used) or sentence recognition score(when sentences used)
- the lowest intensity speech stimulus that an individual can detect at least 50% of the time.
- discrimination means judging two things whether they are same or not ,but this is not done in this test .therefore the term "speech discrimination score' not used now.
- here patient doesn't repeat words ,just a measure of patient's ability to understand speech.
- here Phonetically balanced words(PB) used=single syllable words=pin,bus
- phonetically balanced means that the distribution of phonetic elements in list of words approximates the distribution found in everyday conversations.
- list of 50 words given & then the number of correctly heard words multiplied by 2 to get score.
- done at supra-threshold level i.e, at 30-40dB above SRT.
- in normal people & those with conductive deafness have a high score of 90-100%.
| 90-100% | within normal range |
| 75-90% | slight difficulty |
| 60-75% | moderate difficulty |
| 50-60% | poor discrimination |
| <50% | very poor |
PB max: performance intensity function for PB words.
- here PB scores are taken against several levels of speech intensity at 30-40dB above SRT(suprathreshold level) & maximum score (PB max) is obtained & also note the intensity at which it is obtained.
- this is used clinically to set volume of hearing aid.
Rollover phenomenon: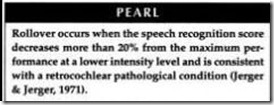
- defined as the decay of the speech discrimination score (greater than 20% change) with increased stimulus intensity,
- When present, this finding is indicative of a retrocochlear lesion
- When the ear with a damaged nervous system is stimulated with a very loud sound, the nerves may be unable to handle the increased signal load. Consider this analogy. If you injured your arm, you might be able to lift a small weight, but would be unable to lift a heavy weight. Similarly, the damaged VIII nerve may be able to transmit a conversational level speech signal, but “tire out” when faced with the demand of sending strong, sustained messages.
Impedence audiometry:::Acoustic immittance.Immittance is a term derived from the terms for two inversely related processes for assessing middle ear function, impedance and admittance. Impedance is the resistance to the flow of acoustic energy. Admittance is the ease of which acoustic energy can flow. A middle ear with low impedence (high admittance) more readily accepts acoustic energy, whereas a middle ear with high impedence (low admittance) tends to reflect energy consists of -
- tympanometry
- acoustic reflex measurements
- The primary purpose of impedence audiometry is to determine the status of the tympanic membrane and the middle ear.
- The secondary purpose of this investigation is to evaluate the acoustic reflex pathway which include the 7th and 8th cranial nerves and the brain stem.

principle:
- when a sound strikes tympanic membrane ,some of the sound energy is absorbed while rest is reflected.A stiffer membrane would reflect more sound energy than a compliant (loose) one.
- so by changing the pressure in a sealed external ear canal & then measuring the reflected sound energy ,we measure the compliance or stiffness of tympano-ossicular system & thus find the healthy or diseased status of middle ear.
- The maximum compliance occurs when the pressure of the external auditory canal and the middle ear becomes equal.
- Only at this pressure maximal acoustic transmission occur through the middle ear & minimum sound energy is reflected back.
Tympanograms:
- A tympanogram is a graphic representation of the relationship of external auditory canal air pressure to impedance
- Pressure in the external auditory canal is varied from -200 daPa(decaPascal=mmH2O) through +200daPa while monitoring impedance
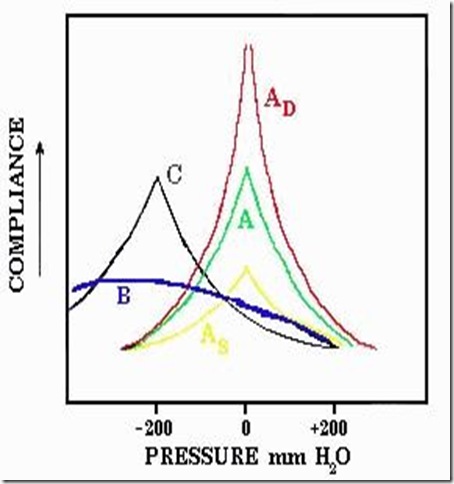
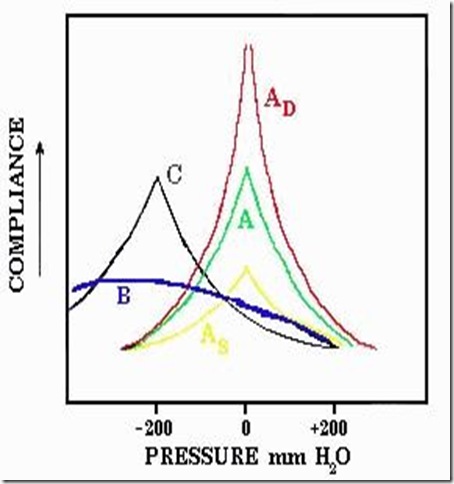
The Jerger system is the most commonly used classification system for tympanograms
- Type A. The peak compliance occurs at or near atmospheric pressure indicating normal pressure in the middle ear. There are three subgroups. Compliance peak is -150 to +100 daPa
- A - normal shape reflects a normal mechanism .immittance is 0.2-2.5 millimhos(unit of conductance)
- AD - A deep curve with a tall peak indicates an abnormally compliant middle ear, as seen in ossicular dislocation or erosion, or loss of elastic fibers in the tympanic membrane. immittance is less than 0.2 mmhos
- AS - A shallow curve indicates a stiff system, as in otosclerosis. immittance is more than 2.5 mmhos
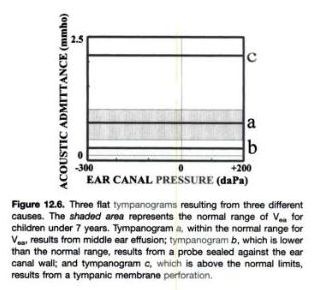
- Type B - No sharp peak, with little or no variation in impedance over a wide range, usually secondary to non-compressible fluid in the middle ear (otitis media), tympanic membrane perforation or obstructing cerumen.
This Type B curve must always be interpreted in conjunction with the ear canal volume. Average ear canal volume in children ranges between 0.42 - 0.97 ml, while in adults it ranges between 0.63 - 1.46 ml.
- Type B curve with normal ear canal volume suggests otitis media.
- Type B curve with small canal volume suggests that the ear canal could be occluded by the presence of wax, or the probe of the impedance audiometer has not been properly placed.
- Type B curve with large canal volume suggests that there could be perforation of the ear drum. (so middle ear volume is added up to volume of ear canal)
- Type C - Peak compliance is significantly below zero, indicating negative pressure (sub-atmospheric) in the middle ear space. This finding is often indicative eustachian tube dysfunction. compliance peak is less than -150 daPa
note:
Testing for the presence of absence of perilymph fistula:
- Testing implies presence or absence of a fistula (ie, an abnormal opening in the inner ear labyrinthine system).
- This can be indirectly assessed by the presence of intense giddiness along with nystagmus when the external canal pressure in increased by increasing the probe pressure. This sign is also known as the Hennebert's sign. This sign is manifested only in the presence of perilymph fistula.
Testing function of eustachian tube:
- A negative or positive air pressure is created (-200 to +200) in middle ear & person is asked to swallow 5 times in 20 sec.
- the ability to equate the pressure indicates normal tubal function.
- also used to test patency of grommet placed in tympanic membrane in cases of serous otitis media.
Physical volume of ear canal:(Equivalent ear canal volume)Includes the volume between
- probe tip(of impedence audiometer) & tympanic membrane ,if tympanic membrane is intact. (or)
- volume of ear canal & middle ear space if tympanic membrane is perforated.
method:
- it is derived from acoustic admittance of volume of air medial to probe.
- Under reference conditions ,a given volume of air has a known acoustic admittance, which can be used to calculate the equivalent volume of air.
- eg;when a 226Hz probe tone is used ,1cubic cm of air has admittance of 1acoustic mmho under standard atmospheric conditions.
- so, if admittance of air b/w probe & tympanic membrane is 1.5 acoustic mmho ,then equivalent volume is 1.5 cubic cm.
Average ear canal volumes for children are 0.42-0.97 mL. Average adult volumes are 0.63-1.46 mL.
Used in case of Type B tympanograms(flat) to know the cause:
- Type B curve with normal ear canal volume suggests otitis media.
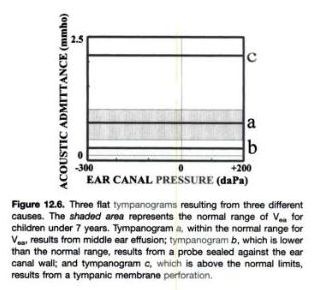
- Type B curve with small canal volume suggests that the ear canal could be occluded by the presence of wax, or the probe of the impedance audiometer has not been properly placed.
- Type B curve with large canal volume suggests that there could be perforation of the ear drum. (so middle ear volume is added up to volume of ear canal)
Static compliance:
- Measure of middle ear mobility.
- it is measures in equivalent volume in cc's, based on 2 volume measurements.
- C1= made with tympanic membrane in position of poor compliance with +200 mmH2O in external canal.
- C2= made with tympanic membrane at max compliance
C1-C2= Static compliance, which cancels out the compliance due to column of air in external canal.the remainder is compliance due to middle ear mechanisms.
static compliance is low when value is less than 0.28cc & high when more than 2.5cc
- its major contribution is to differentiate b/w fixed middle ear & middle ear discontinuity.
Acoustic reflex:
principle:
- Contraction of the stapedius muscle occurs with loud sounds, producing a measurable change in compliance.
- When the stapedius muscle contracts in response to a loud sound, that contraction changes the middle ear immittance. This change in immittance can be detected as a deflection in the recording.
- A significant change in middle ear immittance immediately after the stimulus is considered an acoustic reflex.
- A stapedial muscle contraction in response to an intense signal occurs bilaterally in normal ears with either unilateral or bilateral stimulation. This reaction occurs because the stapedial reflex pathway has both ipsilateral and contralateral projections

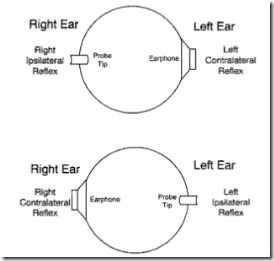
we should first know a few basic terminology used here,
- the immittance change caused by stapedius muscle contraction is measured in the ear containing the probe tip --this is PROBE EAR.
- the ear receiving the stimulus to activate the reflex is --STIMULUS EAR.
- either ear can be stimulus ear --i.e, the stimulus can even originate from the probe tip as well as from the ear phone on the opposite ear.
- Absent reflex means even 125dB of sound doesn't elicit contralateral reflex.
- Elevated reflex : the patient's threshold is compared to respective 90th percentiles that apply to his hearing threshold for the frequencies tested.If ART falls above the 90th percentile it is considered elevated.
- Ipsilateral or uncrossed acoustic reflex: here the stimulus is presented to the probe ear ,which is the same ear in which immitance change is measured.
- Contralateral or crossed acoustic reflex: here the reflex is measured in the ear with probe tip ,but stimulus is given to opposite ear.
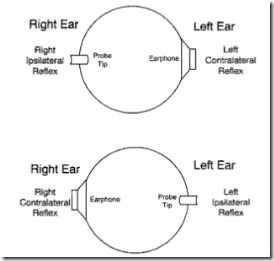 "right contralateral acoustic reflex" means stimulus is in right ear & probe in left ear.
"right contralateral acoustic reflex" means stimulus is in right ear & probe in left ear.
- "left contralateral acoustic reflex" means stimulus is in left ear & probe in right ear.
- Probe ear principle:acoustic reflexes are usually absent when there is conductive pathology in probe ear.
- stimulus ear principle: a conductive disorder in the stimulus ear reduces the stimulus level reaching the cochlea by the amount of air-bone gap,As a result ART is elevated by the amount of air-bone gap.
- 2 basic acoustic reflex tests:
- acoustic reflex threshold(ART)--lowest stimulus which produces reflex
- acoustic reflex decay--measure of how long reflex lasts when stimulus is kept for a period of time
ART:
- Acoustic reflex thresholds generally are determined in response to stimuli of 500, 1000, 2000, and 4000 Hz. For screening purposes, or for a general check of the pathway's integrity, usually test at 1000 Hz.
- Range of ART :loud sound 70-100dB above threshold of hearing of that particular ear is used
- The greater the hearing loss, the higher the acoustic reflex threshold for conductive hearing loss.
- For sensorineural hearing loss, acoustic reflex thresholds may be within the normal range, particularly for mild-to-moderate hearing losses with recruitment.
Absent(means even 125dB of sound doesn't elicit contralateral reflex) in:
- Reflexes usually are absent or cannot be recorded if the patient has type B tympanograms; therefore, acoustic reflexes generally are not tested in these ears.
For example,
- if the ear canal is occluded with cerumen, a type B tympanogram with low volume will be recorded. In this case, acoustic reflexes cannot be measured because middle ear immittance is not being measured. (Cerumen blocks the signal.)
- For a type B tympanogram with normal volume (as in otitis media) no pressure peak for immittance is obtained. The pressure between the ear canal and middle ear are not equilibrated, and acoustic reflexes cannot be recorded.
- For a type B tympanogram with high volume (as in the presence of patent pressure equalization tubes or perforated tympanic membranes), an open exchange of air occurs between the ear canal and middle ear; thus, any contraction of the stapedius muscle cannot be measured.
2. In the presence of severe-to-profound sensorineural hearing loss in the stimulated ear, acoustic reflexes may be absent secondary to insufficient stimulation.
3. Similarly, a conductive component may attenuate the signal intensity, preventing sufficient stimulation in the stimulated ear or precluding a clear response in the recording ear.
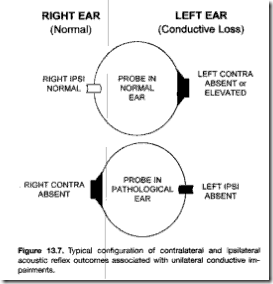
Typical patterns for the interpretation of acoustic reflex abnormalities are as follows:
With unilateral conductive deafness:
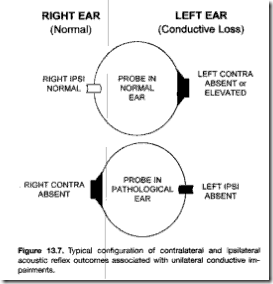
- In the given image ,right contralateral reflex absent or elevated (due to probe principle)
- but left ear ipsilateral absent (due to both probe ear & stimulus ear principles)
So in ipsilateral both principles are operative (ie,stimulus is attenuated due to conductive disorder & even immitance change cannot be measured due to conductive disorder)
Due to this double effect ipsilateral acoustic reflex are so sensitive to conductive disorder.
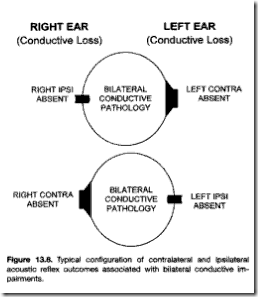
Bilateral conductive disorder:
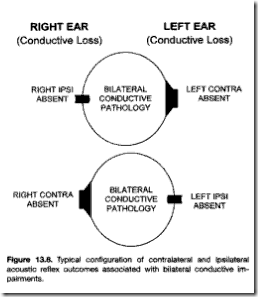
- both contra & ipsilateral reflexes absent in both ears.
Acoustic reflex decay test (adaptation):
- it is measure of how long the response lasts if stimulus is kept on for a period of time.
- The acoustic reflex decay test is used to assess the integrity of CN VIII. Using a stimulus of either 500 or 1000 Hz, a contralateral continuous tone is presented for 10 seconds at a stimulus level 10 dB above the acoustic reflex threshold for that stimulus frequency in that ear. This suprathreshold acoustic reflex then is recorded over the 10-second stimulation period. If the amplitude of the recorded deflection on the screen decreases by 50% or more within 10 seconds, the test is considered positive.
- In some cases of muscular or neuromuscular disorder, tone decay results also may be positive secondary to muscle fatigue.
- along with ART (absent or elevated),acoustic reflex decay is used to detect retro-cochlear disorder
useful in:
- test hearing in infants & young children - since it is objective test
- find malingers- a person who feigns total deafness & doesn't give any response on PTA ,but shows +ve stapedial reflex is malingerer.
- detect cochlear pathology - presence of stapedial reflex at lower intensities like 40 -60 dB than usual 70dB indicates recruitment & thus cochlear type hearing loss
- lesions of facial nerve- absence of reflex when hearing is normal indicates lesion of facial nerve proximal to nerve to stapedius.
- lesion of VIIIth nerve- Acoustic reflex decay test
- lesion in brain stem:ipsilateral reflex present but contralateral absent indicates lesion is in crossed pathways in brain.
Bekesy audiometry:A subject-controlled auditory threshold testing procedure.method:
- the patient has to press a button
- the button controls a motor ,which in turn controls attenuator & a pen.
- patient is told to hold button down when he can hear a tone & release it when he cannot.
- holding the button causes the intensity to fall & releasing to rise.intensity change 2.5dB/sec
- this course of events will cause the level of of tone to rise & fall around the patient's threshold.
- the pen tracks the level of of tone on a paper resulting in zigzag pattern around the patient's threshold.
- the width of the zigzags is EXCURSION WIDTH & the patient's threshold is midpoint of these thresholds.
Conventional Bekesy audiometry:
Bekesy audiograms are obtained either
- one frequency at a time(fixed frequency Bekesy audiometry):one frequency for a given period of time.
- test frequency changes from low to high.(sweep frequency Bekesy audiometry):test tone increases smoothly from 100 to 10,000Hz at rate of 1 octave/sec
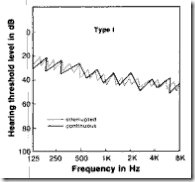
Each Bekesy audiogram is obtained twice
- once with a continuous tone (CONTINUOUS TRACING)
- other with a tone that pulses on & off 2.5 times/sec(PULSED TRACING)
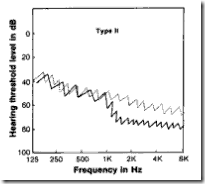
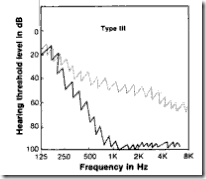
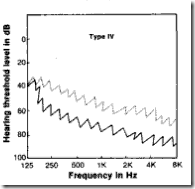
Types of tracing:the shifting of tracing is result of tone decay.
- continuous tracing -(C)
- pulsed tracing-(P)
Modifications of Bekesy audiometry:
Reverse Bekesy tracings:
- Here the sweep of the (C) tracing is from high to low frequency & compared with (P) tracing from low to high.
- advantage is that the patients with sensorineural loss as a result of retrocochlear pathological condition in the region of brain stem had more hearing loss with this procedure.
Bekesy comfort loudness test:
- Patients are instructed to respond to suprathreshold stimuli rather than threshold stimuli.(at a comfortable loudness rather than too loud or too soft)
- reason:retrocochlear disorders initially appear at suprathreshold levels.
We will discuss about the "special tests for hearing assessment" in the next post.