It is one of the most common dermatologic diseases affecting upto 1% of worlds population.

- it is chronic inflammatory skin disorder.
- in Greek it means 'to itch'
for convenience sake we divide the topic into:
- definition
- histopathology
- pathogenesis
- types
- treatment
definition:
Psoriasis is characterized by erythematous sharply demarcated papules & rounded plaques,covered by silvery micaceous scale with a predilection for the extensor surfaces,gluteal cleft,nails and scalp, a frequent positive family history, and is frequently symmetrical and usually chronic.
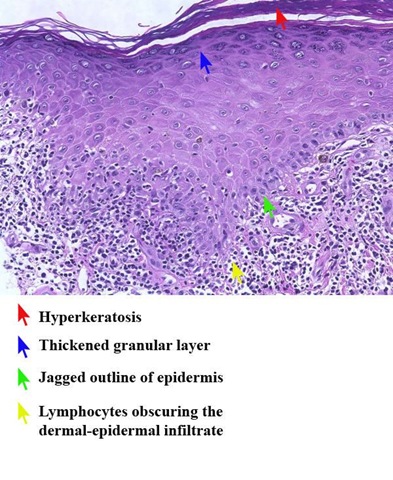
histopathology:

EPIDERMIS-
early changes: The first histopathological change is invasion of the epidermis by neutrophil polymorphs (and maybe a small micro abscess).
changes in established psoriasis:are essentially epidermal.
- The horny layer shows considerable hyper & parakeratosis(nuclei in stratum corneum)
- The granular layer is reduced or absent in active lesions.
- acanthosis(marked epidermal hyperplasia)
- The rete ridges are greatly elongated & often clubbed. They are separated by oedematous papillae, also club shaped
- Mitotic activity is the basal and suprabasal cells are greatly increased.
- Cellular invasion(of neutrophils) takes place, particularly in the suprapapillary region to form the Munro 'micro abscess' which are extruded in the horny layer or they may collect in disintegrated malphigian cells, the cytoplasm of which had been lysed to form the multilocular or spongiform pustule of Kogoj.{The spongiform pustule of Kogoj, one of the most characteristic features of psoriasis is located in the uppermost portion of spinous and granular layers. Here neutrophils lie intercellular in a multilocular pustule in which sponge like network is composed of degenerated and flattened keratinocytes.}
In the DERMIS the main changes consist of papillary oedema, dilatation and tortuosity of the papillary capillaries and a mild to moderate infiltrate of lymphocytes with occasional histiocytes.
pathogenesis:
- Recently, clinical studies provided fairly direct evidence for an involvement of T cells in the pathogenesis of psoriasis .T- lymphocytes release proinflammatory cytokines and lymphokines that stimulate keratinocyte proliferation and induce abnormal epidermal maturation.
- strong association with HLA-Cw*0602 allele(histocompatibility complex)
- TNF(tumor necrosis factor) is a major mediator in pathogenesis.
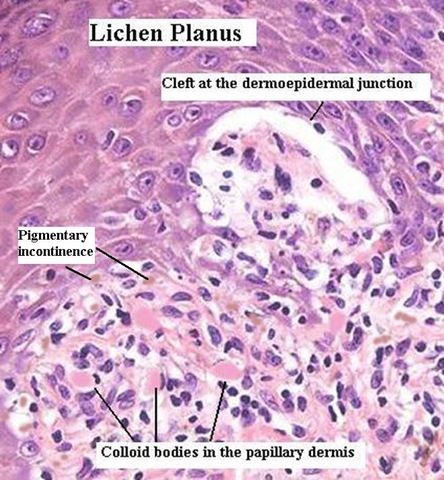
- A further point is that the whole skin is abnormal in psoriasis. Thus in a patient with very active disease if some of the skin that appears not to be involved with psoriasis is scratched or traumatised with a burn or cold then a psoriatic lesion might develop there. This phenomena is referred to as Koebner's phenomena. Koebner's phenomena is also seen in some other diseases like lichen planus & Vitiligo..
- A form of psoriasis, guttate psoriasis comprising small droplet like lesions all over the body, particularly common in early life, appears to follow streptococcal sore throats. Again, like the HLA evidence this all suggests some sort of prominent role for the immune system in the disease.
note:provocation factors-
Psoriasis is marked by periods of remissions and exacerbations. Remissions usually last a few weeks to many years. Both local and systemic provocation factors bring in exacerbations.
- Local Factors: Local injury to the skin produces psoriatic lesions, the well-known Koebner Phenomenon.
- Trauma involving the papillary dermis could be physical, chemical, mechanical, allergic or burns, drug eruptions, dermatitis, lichen planus, miliaria, herpes zoster, chickenpox etc. Koebner phenomenon occurs usually within 7-14 days (ranging from 3 days to 3 weeks)
- Seasonal variations: In most patients, psoriasis worsens during cold weather. High humidity is usually beneficial, whereas sunlight worsens in some but improves in many.
- Pregnancy:In most cases pregnancy induces remissions, though raised levels of progesterone in the latter half of pregnancy can precipitate generalized pustular psoriasis in some.
- Emotional Stress: Psoriasis is well known to be induced, exacerbated, or sustained due to emotional stress. The mechanism is not yet well understood, but neuropsychoimmunological mechanisms are hypothesized. The disease itself could produce a reactive depression, which could further exacerbate the disease.
- Infections:Streptococcal URTI has been shown to exacerbate existing psoriasis and precipitate an attack of acute guttate psoriasis mainly in children.
- Drugs:Many drugs are known to precipitate or exacerbate psoriasis.
- Beta-blockers like propranalol, practalol, and metapralol may induce or exacerbate psoriatic eruption.The eruption usually disappears within 2 to 6 weeks of cessation of the drugs.
- Almost all NSAIDS affect psoriasis adversely.
- Anti depressants like lithium compounds and Trazodone may precipitate generalized pustular psoriasis.
- Too rapid withdrawal of corticosteroid therapy may precipitate pustular or erythrodermic exacerbations of psoriasis.
- Alcoholic beverages affect psoriasis adversely.
- Chloroquine, clonidine, iodides, glibenclamide, and tetracycline are a few other drugs known to exacerbate psoriasis.
types:
Plaque psoriasis(psoriasis vulgaris)is characterized by raised inflamed lesions covered with a silvery white scale. The scale may be scraped away to reveal inflamed skin beneath. This is most common on the extensor surfaces of the knees, elbows, scalp, and trunk.

Guttate(drop shape) psoriasis presents as small red dots of psoriasis that usually appear on the trunk, arms, and legs; the lesions may have some scale. It frequently appears suddenly after an upper respiratory infection (URI).

Inverse psoriasis occurs on the flexural surfaces, armpit, groin, under the breast, and in the skin folds and is characterized by smooth, inflamed lesions without scaling.

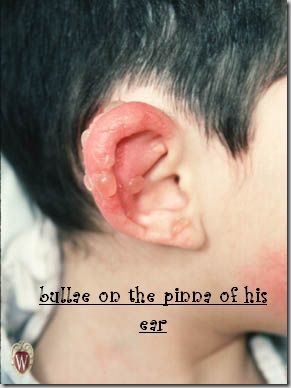
Pustular psoriasis presents as sterile pustules appearing on the hands and feet or, at times, diffusely, and may cycle through erythema, pustules, and scaling. can be localised (on palms & soles) or generalized(characterized by fever, leukocytosis, arthralgia,diffuse cutaneous & mucous pustules,secondary infection ,electrolyte disturbances)

Erythrodermic psoriasis presents as generalized erythema(more than 90% skin), pain, itching, and fine scaling.

Scalp psoriasis affects approximately 50% of patients, presenting as erythematous raised plaques with silvery white scales on the scalp.
Nail psoriasis may cause pits on the nails, which may develop yellowish color(resembles oil drop under nail plate) and become thickened. Nails may separate from the nail bed.


Psoriatic arthritis affects approximately 10% of those with skin symptoms. it is asymmetric inflammatory arthritis most commonly affecting distal & proximal interphalangeal joints.
Oral psoriasis may present with whitish lesions on the oral mucosa, which may appear to change in severity from day to day. It may also present as severe cheilosis with extension onto the surrounding skin, crossing the vermillion border.
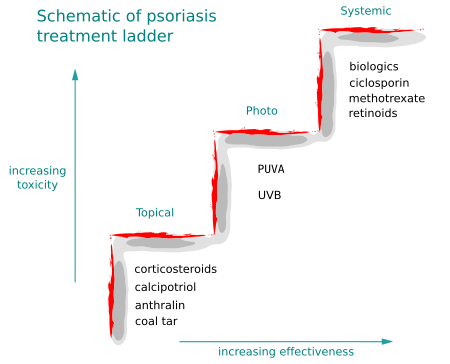
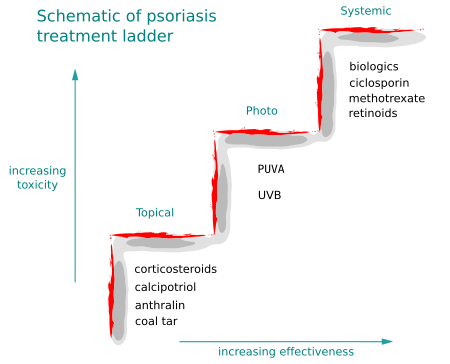
treatment:
topicals:
Topical steroids:
- Topical steroids are the most widely used medications for psoriasis. They are effective, convenient to use and affordable.
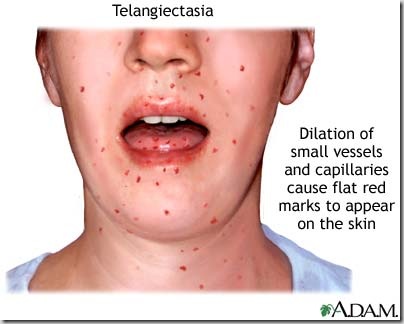
- Most common side effect is cutaneous atrophy. But the atrophy is reversible in most cases if medication is discontinued early. Other side effects are telangiectasia, folliculitis, perioral dermatitis etc.
- Many dermatologists believe that tachyphylaxis and steroid rebound are major limitations of long-term therapy with steroids in psoriasis.
- Treats inflammatory dermatosis responsive to steroids. Decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reversing capillary permeability.
- Triamcinolone acetonide -Has mild potency and is the first DOC for most patients.
- Betamethasone dipropionate -Is a potent topical steroid and is DOC if psoriasis is resistant to milder forms.
- oral steroids should not be used for psoriasis since risk of developing pustular psoriasis if therapy discontinued.
Coal tar
- An inexpensive treatment that is available over the counter in shampoos or lotions for use in widespread areas of involvement. It is particularly useful in hair-bearing areas.
- Antipruritic and antibacterial that inhibits deregulated epidermal proliferation and dermal infiltration. Does not injure the normal skin when applied widely and enhances the usefulness of phototherapy. Generally is used as a second-line drug therapy due to messy application, except for shampoos, which may be used and rinsed at once.
- Goeckerman regimen. Once or twice daily, crude coal tar is applied and then removed before the patient is exposed to total body UVB light. This is followed by a cleansing bath or shower to remove the residual tar and scales.
- Adverse reactions:
- Staining and odour of the tar, lessened in newer preparations
- Folliculitis (Commonest)
- Primary irritant reaction if used in areas like face, genitalia and flexures.
- Carcinogenecity: In cases of prolonged usage with UV light therapy.
Contraindications:
1. Erythrodermic Psoriasis
2. Generalized Pustular Psoriasis
3. Pre-existing folliculitis/ severe acne
Dithranol/Anthralin:
- It is a synthetic derivative of chrysarobin, a tree bark extract. Since it is an unstable product, combining with salicylic acid stabilizes it.
- adverse:highly irritant especially on the head and neck areas and stains linen irreversibly.
- The Ingram regimen
The Ingram regimen combines anthralin paste, a coal tar bath and UV exposure. Anthralin is applied to lesions as a thick paste. Once the anthralin is removed, the patient is then exposed to UV and may also take coal tar baths. Generally, a patient using the Ingram regimen in the hospital or day treatment program will require three weeks of therapy, clearing in an average of 20 days.
Vitamin D-3 analog (calcipotriol)
- Used in patients with lesions resistant to older therapy or with lesions on the face or exposed areas where thinning of the skin would pose cosmetic problems.
- Mechanism of action is through induction of terminal differentiation of keratinocytes and inhibition of T cell proliferation.
- It is widely used in chronic plaque psoriasis alone or in combination with potent steroid
- The lesions and surrounding uninvolved skin may be irritated following treatment; if this happens, discontinue treatment; it may transiently but reversibly elevate serum calcium; discontinue if increase is outside the normal range
retinoid (tazarotene)-
- A retinoid prodrug that is converted to its active form in the body and modulates differentiation and proliferation of epithelial tissue and perhaps has anti-inflammatory and immunomodulatory activities. May be the DOC for those with facial lesions who are not at risk of pregnancy.
- adverse:
- May cause a feeling of burning or stinging
- caution patients to take protective measures against exposure to ultraviolet or sunlight, since photosensitivity may result
phototherapy:
There are two main forms of phototherapy, that based on ultraviolet B therapy, most commonly given as narrowband or TLO1 therapy, and PUVA therapy. PUVA stands for psoralen + UVA.
PUVA-
- It consists of ingestion of Psoralen in the dose of 0.6-mg/kg body weight on alternate days and followed in 2-3 hours later by UV radiation for graded periods.
- The commonly used psoralens are 8-methoxy psoralen and 4,5,8 trimethoxy psoralen.
- PUVA therapy affects DNA synthesis and proliferation of cells in psoriatics by 2 mechanisms:
- An anoxic reaction that affects cellular DNA with the formation of photo adducts.
- An oxygen dependent reaction where free radicals and reactive oxygen formed may damage the membrane of lipid per oxidation and induce activation of mediators of the eicosanoid system.
- PUVA therapy also reduces the chemo tactic activity of the psoriatic leukotactic factor.
- Topical PUVA has been tried in the form of PUVA bath. Trimethoxy psoralen 50mg in 100ml ethanol is added to a 150-litre bath. Patient is allowed to bath for 15 minutes and then exposed to UVA at 290-320 nm. Photosensitivity is achieved immediately after this bath is 15 times greater than after oral psoralen and side effects like nausea, headache can be minimized by PUVA bath.
- Side effects of PUVA therapy:
- Nausea, vomiting, headache, vertigo, erythema, pruritus, blistering
- Koebner phenomenon
- Hypertrichosis, hyper pigmentation
- Lichenoid eruption
- Photo-onycholysis
- Premature ageing of skin, Cataract formation
- Increased incidence of skin cancers etc.
Ultraviolet B
The main wavelength in natural light that appears to be effective is ultraviolet B (despite most natural light being UVA). Experiments have shown that particular wavelengths of ultraviolet radiation between 310 to 315 nanometers. A particular lamp has been developed with a peak exposure within this area (so called narrowband or TLO1 lamp) and this is highly effective for psoriasis. It is however not as effective as PUVA treatment but is administered similarly on a twice weekly basis. In general most patients would be treated with TLO1 first and if this failed or the remission induced was not good they would be treated with PUVA on the following occasion
note:UV therapy is contraindicated in patients taking cyclosporine & used with care in immunocompromised since increased risk of developing skin cancers.
Systemic Treatments
In general the rule is start with topical agents, move onto phototherapy and if this fails consider systemic agents.
this includes biologics(targeted drugs) & 3 other drugs-
methotrexate:
Methotrexate -antimetabolite.It acts on 's' phase of cell cycle
Contraindications:
- Absolute: Pregnancy, Lactation
- Relative: Decreased renal function, hepatic disease, severe hematological abnormalities, alcoholism, child bearing age (12weeks before conception: should be stopped in both sexes), active infectious diseases, h/o potentially serious infection that could be reactivated, immunodeficiency syndromes, unreliable patient.
- Oral dose: single, or more commonly 3 divided doses at 8 am, 8 pm, 8 am once a week (Rationale: Presumed cell kinetics in psoriasis cell cycle shortened from 19 days in normal to 37.5 hours in psoriatic epidermis.) i.e,3 doses taken for 2 days.remaining 5 days folic acid is taken(to prevent toxicity to normal body cells)
- Initial dose-5-10 mg stat: CBC(complete blood count), LFT(liver function tests) after 7 days.
- If Okay, escalate dose to 2.5-5mg per week to get reasonable benefit without toxicity.
- 10-12.5 mg/week on an average gives maximum benefit.
Adverse Effects:
- Hepatotoxicity: Regular monitoring to detect
- Pulmonary Toxicity: Pneumonitis, Pulmonary Fibrosis
- Hematological Effects: Myelosupression
- Gastrointestinal: Nausea, diarrhoea, ulcerative stomatitis, anorexia, vomiting
- Potent Teratogen
- Other: alopecia, fatigue, phototoxicity, headache, and dizziness.
Retinoids are synthetic or natural analogues of vitamin A.
The 3 main ones are:
1. Isotretinoin (13 cis retinoic acid)
2. Etretinate
3. Acitretin
Acitretin is an active metabolite of Etretinate. Etretinate is an ester and acitretin a corresponding free acid. Its great advantage over etretinate is its decreased lipophilicity, which results in elimination half-life of 50 hours as opposed to more than 80 days for etretinate. However the clinical efficacy and side effects are similar to etretinate.
The mode of action of retinoids is not fully established. It seems to induce a better maturation in keratinocytes and to reduce the neutrophil chemotaxis in pustular psoriasis.
Indications:
- 1. Generalized Pustular Psoriasis: Considered to be the drug of choice.
- 2. Psoriatic erythroderma.
- 3.Severe psoriasis vulgaris, where other modalities have either failed or are contraindicated.
- 4.Palmo-plantar pustular psoriasis.
Dose:
0.5-1 mg/kg/day is the usual initial dose of etretinate. Maintenance dose of 0.5 to 0.75mg/kg/day. Remission may take anywhere from 12-24 weeks. Relapses are very common following discontinuation of treatment.
Acitretin- an optimum dose of 50mg daily (mean 0.66mg/kg/day) is recommended.
Contraindications:
1.Women of child bearing age, unless the psoriasis is unresponsive to other therapies or where clinical condition contraindicates the use of other regimens.
In such cases the following precautions are to be strictly adhered to:
a. Has received both oral and written warning of hazards of taking acitretin
b. Should be on reliable form of contraception
c. Should have negative serum and urine pregnancy test done at least 1 week prior to beginning treatment.
d. Treatment should be started on the 2nd or 3rd day of next normal menstrual period.
2. Pregnancy
3. Children
4. Active liver disease
5. Pre-existing hyperlipidemia
Side Effects:
Almost 99% of patients receiving retinoids develop some sort of side effect.
- It is highly teratogenic.
- The retinoids are lipophilic and are retained in the body for a considerably longer period of time. So women receiving the drug should avoid pregnancy for a period of 3 years.
- Lipid abnormalities in the form of increased serum triglycerides and cholesterol may necessitate discontinuation of therapy. In mild cases, the abnormality may be alleviated by concomitant administration of fish oils.
- Liver enzyme elevation, hepatitis and jaundice
- Radiological spinal changes including anterior spinal ligament calcification, osteophytes, disc abnormality, DISH (diffuse idiopathic skeletal hyperosteosis) can occur
- In children, premature closure of epiphyses, growth retardation and hyperosteosis can occur
- Dryness of the lip, nose, mouth, eyes, throat with peeling of skin, exfoliative cheilitis, uveitis, balanitis, gingivitis, corneal ulceration, burning sensation of skin, atrophy of skin, alopecia, epistaxis, increased bruising, generalized erythema
- Purulent paronychia may necessitate stopping of therapy.
- Pseudotumour cerebri is not uncommon
Drug Interactions:
- Do not give tetracyclines along with retinoids (pseudotumour cerebri)
- No supplementation with vitamin A
- Concommitant methotrexate increases hepatotoxicity
- Ethanol should not be given along with acitretin because it is converted to etretinate
Cyclosporine:calcineurin inhibitor
It is indicated for the treatment of adult non immuno-compromised patients with severe recalcitrant psoriasis who have failed to respond to at least one systemic therapy or in patients for whom other systemic therapies are contraindicated or cannot be tolerated.
adverse effects-
renal dysfunction, hypertension, hyperkalemia, hyperuricemia, hypomagnesemia,hyperlipidemia,increased risk of malignancy.
biologics:
| drug | mechanism | route | adverse effects |
| alefacept | anti-CD2 | IM | lymphopenia |
| etanercept | anti-TNFalfa | SC | neurologic events |
| efalizumab | anti-CD11a | SC | thrombocytopenia,hemolytic anemia |
| adalimumab | anti-TNFalfa | SC | hypersensitivity reactions,neurologic events |
| infliximab | anti-TNFalfa | IV | hepatotoxixity,neurologic events,hypersensitivity reactions, |
note:
- adverse effects shared by all biologics-potential for increased malignancies,serious infections.
- adverse effects shared by all anti-TNFalfa agents are-may worsen congestive heart failure.
- Up to 20% of patients with psoriasis have extensive skin disease, and etanercept may be the biological agent of choice for these patients.
in pregnancy:
Topical corticosteroids, calcipotriol, broad band UVB used.
- Topical corticosteroids have been widely used during pregnancy, although intrauterine growth retardation was reported in an infant whose mother applied 40mg/day of topical triamcinolone beginning at 12 weeks of gestation.
- Calcipotriene is approximately 6% absorbed when the ointment form is applied to psoriatic plaques and is likely safe in pregnancy for the treatment of localized psoriasis
- Broadband ultraviolet B phototherapy is considered the safest therapy for extensive psoriasis during pregnancy, although overheating during treatment should be avoided.
- PUVA is a potential teratogen because it is known to be mutagenic and to induce sister chromatid exchanges. However, adverse outcomes have not been reported in studies of women exposed to PUVA during pregnancy.
- Methotrexate and acitretin are both in pregnancy category X. Methotrexate can be used in women with childbearing potential who are using effective contraception. Pregnancy should be avoided for at least one ovulatory cycle after this medication is discontinued. Acitretin should not be prescribed for women of childbearing potential.
- There are limited data on the safety of biologics used for the treatment of psoriasis during pregnancy