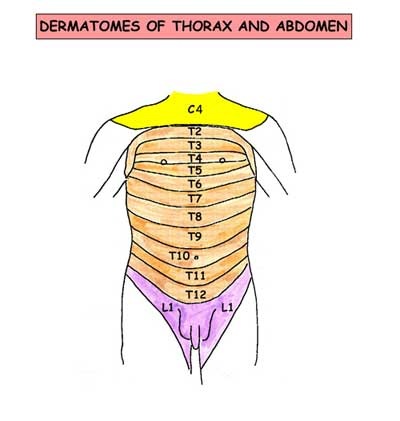
so pain in gut viscera is referred to their respective dermatomes ,especially at midline & only in severe cases to sideways
Gall bladder pain:
pain along T7 -T9 segments(right hypochondrium to inferior angle of right scapula)
Diaphragm pain:
along C3,4,5 (pain over shoulder)
Urinary organs pain:
along dermatomes L1 & L2(along genitofemoral nerve)
retroperitoneal visceral pain:
pain is felt in back in addition to referred pain on sensory dermatomes
eg-pain in pancreas.
Nature of pain:varies with nature of disease
- continous pain -inflammatory
- colic (intermittent ,gripy ,in wave form) -spastic conditions.
Dysfunction:
In gut disease it results in Dyspepsia -it is a very vague term literally meaning -difficulty in digestion.
patient may complain of -
- lack of appetite
- nausea
- vomiting
- diarrhea
- constipation ,etc
now let us consider each abdominal organ dysfunction separately.
stomach:
- mild dysfunction results in -anorexia
- moderate - nausea
- severe - vomiting
note:stomach has property of receptive relaxation(to receive food from oesophagus) & propulsive expulsion(to expel into duodenum).
- bloating sensation(due to absence of receptive relaxation)-patient feels heavy even with small amount of food ,since there is no relaxation of stomach.
small bowel:
colon:
- altered bowel habits
- discharge of mucus per rectum
liver:jaundice
urinary organs:disturbance in micturation
female reproductive organs:menstural disturbance.
Modified presentation
due to exaggerated sympathetic response to some organs, especially stomach.
let me explain it to you with an example:
- suppose small bowel is diseased ,so to recover it needs rest from its usual work. so for this to occur the stomach causes symptoms like anorexia , nausea ,vomiting .so as a result the person wont like to eat anything & thus his small bowel gets some rest & it recovers fast.
- suppose the stomach doesn't make these manifestations to occur ,then the person keeps on eating & there is no rest for small bowel & its condition detiorates.
- Hence stomach acts as a BIG BROTHER of abdomen.
- sometimes its response is greater than the diseased organ & disease is mistaken as gastric disorder. so you should keep in mind about the other possibilities of each presentation.
presentation as lump:
site of lump indicates site of its origin unlike pain.
now lets go to clinical examination:
- detailed history taking
- general examination
- abdominal examination
- examination of scrotum ,supraclavicular nodes & spine.
detailed history taking:
points to be enquired
pain:
- site( initial & present)
- nature
- aggravating & relieving factors
- relation to food ,vomiting ,defecation
- periodicity
presenting features of dysfunction of viscera
- anorexia ,nausea ,vomiting(stomach)
- diarrhea(small bowel)
- altered bowel habits .mucus/ blood in stools (colon)
- frequency ,difficulty in micturation ,haematuria (urinary organs)
- menstural disturbance (female genital tract)
- jaundice(liver)
- any general disturbance like fever ,loss of weight (T.B. ,malignancy ,etc)
lump:
- initial site of appearance
- rate of growth
- associated with pain or not
- preceding history of abdomen disease.
general examination.
PICCKLE ,heart & lung sounds.
P-pallor(check lower palpebral conjunctiva)
I-icterus/jaundice(upper bulbar conjunctiva)
C-cyanosis(tongue)
C-clubbing
K-koilonychia
L-lymphadenopathy
E-edema
abdominal examination
Inspection:
skin & subcutaneous tissue:
- abdominal lump
- superficial engorged veins:
| features | portal obstruction | inferior vena cava obstruction | superior vena cava obstruction |
| position | situated around umbilicus (caput medusa) | on sides of abdomen | on sides of abdomen |
| direction of blood flow | away from umbilicus | from below upwards | from above downwards |

note:direction of blood flow is known by following technique-
- two index fingers of both hands are placed close together on engorged vein below umbilicus
- portion of vein is emptied by milking it with one of the index fingers
- remove the upper finger, the vein remains collapsed if flow is from below upwards .vein fills quickly if flow is from above downwards.
- repeat the same process of emptying the vein , but now remove the lower finger.the vein remains collapsed if flow is from above downwards .vein fills quickly if flow is from below upwards.
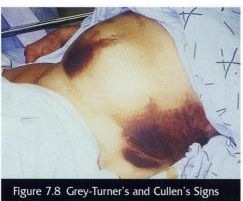
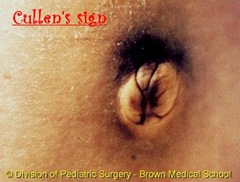
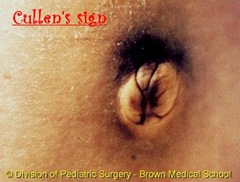
Cullen's sign & Grey-Turner's sign:
- Cullen's sign is ecchymosis (puplish blue discolouration) of the skin around the umbilicus.
- Grey-Turner's sign is ecchymosis in flanks.
- mainly associated with hemorrhagic pancreatitis (in 1 to 2 % cases seen)
- (typically after 2 to 3 days after acute pancreatitis)
- represent retroperitoneal hemorrhage that has dissected through fascial planes to skin
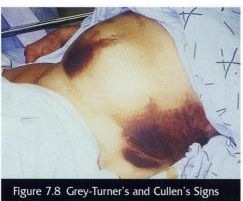
also seen in:
- ruptured ectopic pregnancy ,severe trauma
- leaking or ruptured abdominal aortic aneurysm
- any condition associated with bleeding into retroperitoneal space
It is caused by pancreatic enzymes that have tracked along the falciform ligament and digested subcutaneous tissues around the umbilicus.
scar:
- linear scar -healing by primary intention
- irregular scar -indicating wound infection
- keloid , hypertrophic scar.
hard subcutaneous nodules near umbilicus:Sister Mary Joseph Nodule

- She was first to notice that a 'nodule' in the umbilicus was often associated with advanced malignancy
- Presents as firm, red, non-tender nodule
- Results from spread of tumour within the falciform ligament
- 90% of tumours are adenocarcinomas
- Commonest primaries are stomach and ovary
- Primary tumour is almost invariably inoperable
abdomen distention:5F's
- fetus
- faeces
- flatus(gas)
- fluid
- fat
note : among these only in fat distention ,umbilicus is deeply inverted & in others it is flat or everted.(reason:umbilicus is a scar ,which is bound to linea alba & when fat increases, it fills around the umbilicus as subcutaneous fat & thus causes raising of level of skin around it)
umbilicus:
tanyol's sign:umbilicus is displaced upwards by swelling arising from pelvis or downwards by ascites.
any swelling on one side of abdomen will push umbilicus to opposite side.
movements:
respiratory - localised limitation indicates subjacent inflammation
peristaltic -
| observed in | pyloric stenosis | obstruction in small bowel | obstruction in large bowel |
| features | rounded prominence will be seen travelling slowly from left costal margin to right | ladder pattern | opposite movement to that of pyloric stenosis |
pulsatile:
- aortic aneurysm - expansile pulsation
- tumor in front of abdominal aorta - transmitted pulsation
palpation:
tenderness(pain on touch):
| disease | tender spot location |
| gastric ulcer | mid-epigastrium below xiphoid process |
| duodenal ulcer | 1&1/2 inch to right of midline on transpyloric plane |
| cholecystitis | - Palpation under the right costal margin whilst asking the patient to breathe in causes pain as the inflammed gallbaldder touches with the palpating hand.(Murphy's sign)
- cartilage of right 8th rib becomes tender
- hyperaesthesia below the right scapula, called Boas' sign.
|
| appendicitis | McBurney's point(McBurney's point refers to the location of the base of the appendix. It lies one third of the way along an imaginary line drawn from the anterior superior iliac spine to the umbilicus.)-this is McBurney's sign. |
rigidity & guarding(stiffness):in both there is reflex contraction of abdominal wall
- in rigidity ,it is present at rest &
- in guarding it appears due to provocation from pressure of examining fingers
lump:
- character(consistency)
- its anatomical plane(intra-abdominal or parietal) :
abdominal muscles are made taut by asking patient :
- to raise his shoulders from bed with arms folded on his chest 'the rising test'
- to raise both extended legs from bed -'leg lifting test'(carnett's test)
- try to blow out with nose & mouth shut.
results:if swelling is-
- parietal -swelling will become more prominent & will be freely moveable over the taut muscle.
- parietal but fixed to abdominal muscles = swelling will not be moveable over the taut muscle.(eg: recurrent fibroid of paget & haematoma in rectus muscle)
- intra-abdominal-disappears or becomes smaller.
note:if swelling moves vertically with respiration it is intra-abdominal.
Palpation of abdominal organs:
- stomach
- liver
- spleen
- gallbladder
- kidney
- pancreas
- colon
stomach:
- normally cannot be palpated.
- in cases of pyloric stenosis-look for
- visible peristalsis
- succussion splash
- the stomach becomes distended with fluid (ingested liquid ,saliva & gastric fluid) when the pylorus is obstructed by tumor or cicatricial stenosis.
- when the diaphragm of stethoscope is placed medial to left costal margin & patient is shaken from side to side by the lower ribcage ,a splashing sound is heard ,that is pathognomic for this condition.

- the test must be carried out after a 4hr fast.(since Succussion splash may be heard in normal subjects for up to 3 hours after a meal).
- A positive succussion splash indicates a hollow area containing both fluid and gas.
- For abdominal examination, the examiner's hand is placed in the area to be examined, a soft pressure is applied, and then the examiner gives short ,sudden ,jerky movements with fingers. This will, if the sign is positive, result in a palpable or audible splash.
- For thoracic examination, auscultates while gently moving the patient side to side on the examining table.
- A thoracic succussion splash is found in a pneumohydrothorax (air and fluid in the chest cavity) or rarely in hemopneumothorax.
lump in pyloric region:
- congenital pyloric stenosis - thick pylorus
- carcinoma - mass is irregular , hard with varying degrees of mobility
- leaking perforation of peptic ulcer - firm ,less mobile ,more tender
{absence of lump by no means excludes carcinoma of stomach}
Liver:
- children upto end of 3 years - palpable
- adults - not palpable
Gall-Bladder:
when distended felt as tense globular swelling projecting downwards & forwards from below liver just lateral to outer border of right rectus muscle.
Courvoisier's law
- It states that, in the presence of jaundice, an enlarged gallbladder is unlikely to be due to gallstones; rather carcinoma of the pancreas or the lower biliary tree is more likely.
- Gallbladder distension has been thought to occur because the distal malignant obstruction leads to chronically elevated intraductal pressures. This contrasts with obstructions caused by stones, which are associated with chronic cholecystitis and fibrosis of the gallbladder wall, which precludes distension.
- In addition, stones may cause only partial obstructions (related to a "ball-valve" action of the stone) leading to less consistent intraductal pressure elevations, and less gallbladder dilatation.
Exceptions to Courvoisier's Law
1. Oriental cholangiohepatitis
2. Double stone impaction (one in cystic duct, other in Common Bile Duct)
3. a pancreatic calculus obstructing ampulla of vater
4. Mucocele of gall bladder due to an impacted stone at neck of gall bladder.
Spleen:
- spleen must be atleast two times larger than normal size to be detected clinically.
- splenic swelling:sharp anterior border where 1 or 2 notches felt (characteristic of splenic swelling)
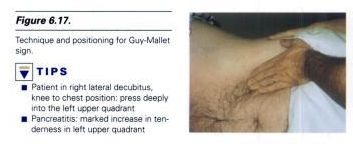
Pancreas:best way to palpate it:
- turn patient to right.
- hips & knees flexed
- left subcostal & epigastric regions deeply palpated.
if tenderness present - indicates pancreatitis (this is Guy -Mallet sign)
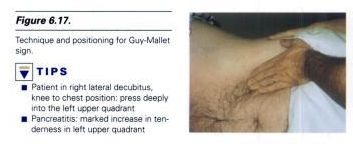
this pain & tenderness often radiates to left shoulder - Kehr's sign
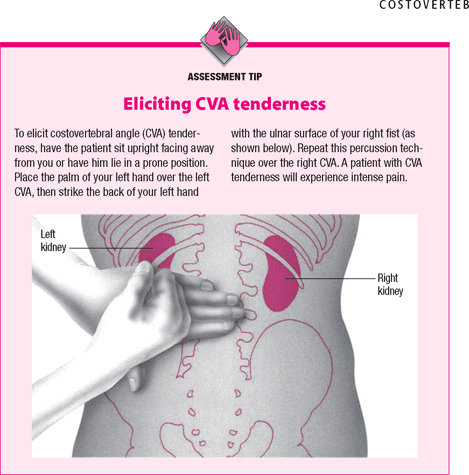
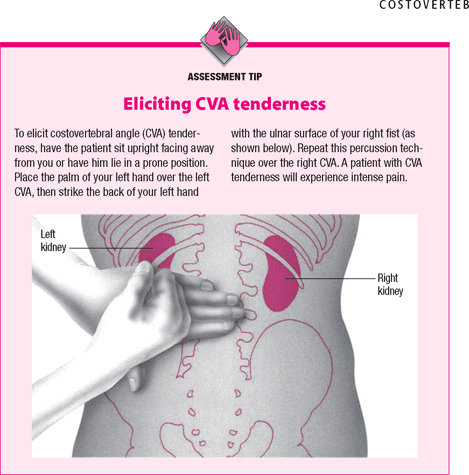
Renal:
renal angle :check this area for signs of renal disease
- An area located on either side of the human back between the lateral borders of the erecter spinae muscles and inferior borders of the twelfth rib, so called because the kidney can be felt at this location.
- check for any dullness ,tenderness ,fullness.
percussion:
evaluate-
- free fluid in abdomen (by shifting dullness)
- presence of gas filled viscus in front of any lump: eg-if anterior to stomach -dull note on percussion.
- if posterior to stomach-resonant note on percussion
- borders of solid organs mapped out by their dull note
| ascites | ovarian cyst |
| resonance | anteriorly | flanks |
| dullness | flanks | anteriorly |
| shifting dullness | present | absent |
Spleen: to evaluate splenomegaly -
Castell's sign -
- percussion in the lowest intercostal space(8th or 9th) in the left anterior axillary line.
- In normals this area is resonant( due to the air-filled stomach or splenic flexure of the colon.)in inspiration and expiration.
- With splenic enlargement this area becomes dull on maximal inspiration.
percussion over traube's space:
- It's a crescent-shaped space, encompassed by the lower edge of the left lung, the anterior border of the spleen, the left costal margin and the inferior margin of the left lobe of the liver.
- Thus, its surface markings are respectively the left sixth rib, the left anterior axillary line, and the left costal margin.

- Underneath Traube's space lies the stomach, which produces a tympanic sound on percussion.
- If percussion over Traube's space produces a dull tone, this might indicate splenomegaly
note:Castell’s has been shown to be superior in sensitivity to other spleen percussion signs as well as palpation, which is not likely useful due to the extreme enlargement necessary to feel the spleen below the costal margin.
auscultation:
• Systolic bruit heard over an artery indicates stenosis of the underlying artery. Systolic bruit may be heard also over very vascular intra-abdominal tumors.
• Venous hum is rarely heard. When present, it is a sign of venous collaterals developed secondary to portal hypertension.
Kenawy's sign:
- seen in splenomegaly due to portal hypertension
- hear a venous hum louder on inspiration with stethoscope placed below xiphoid process
- reason:due to spleen being compressed during inspiration results in engorgement of splenic vein & hum is heard
Left supraclavicular lymph nodes:
enlargement of these group of nodes occurs in carcinoma of stomach - Troisier's sign.
This is end of todays post ,to sum up I will write the important high yield facts here:
- Cullen's sign is ecchymosis (puplish blue discolouration) of the skin around the umbilicus.Seen in hemorrhagic pancreatitis.
- Grey-Turner's sign is ecchymosis in flanks. seen in hemorrhagic pancreatitis.
- Guy -Mallet sign : tenderness present in left subcostal & epigastric regions when deeply palpated.seen in pancreatitis.
- Kehr's sign :pain & tenderness often radiates to left shoulder in pancreatitis.
- Sister Mary Joseph Nodule : a 'nodule' in the umbilicus seen especially in advanced stomach cancer.
- tanyol's sign: umbilicus is displaced upwards by swelling arising from pelvis or downwards by ascites.
- Boas' sign :hyperaesthesia below the right scapula in cholecystitis
- Murphy's sign :Palpation under the right costal margin whilst asking the patient to breathe in causes pain as the inflammed gallbaldder connects with the palpating hand
- Castell's sign - percussion in the lowest intercostal space(8th or 9th) in the left anterior axillary line. causes a dull note in splenomegaly
- Kenawy's sign :venous hum louder on inspiration with stethoscope placed below xiphoid process seen in splenomegaly due to portal hypertension